Vitamin D plays an important role in most diseases, including infectious disease, which is why from the very beginning of the COVID-19 pandemic, I suspected that optimizing vitamin D levels among the general population would significantly lower COVID-19 incidence and death.
Since then, mounting evidence reveals this is indeed the case, as researchers have repeatedly demonstrated that higher vitamin D levels reduce rates of positive tests, hospitalizations and mortality related to this infection.
Vitamin D3 Reduces ICU Admissions and Mortality
Most recently, a Spanish study1,2 (which has yet to undergo peer-review) found giving supplemental vitamin D3 (calcifediol) to hospitalized patients with PCR-confirmed COVID-19 reduced ICU admissions by 82% and mortality by 64%.3 People who already had higher vitamin D at baseline were 60% less likely to die.
The study included 930 patients, 551 of whom received vitamin D3 — 532 micrograms on the first day of admission followed by 266 mcg on days 3, 7, 15 and 30. The remaining 379 patients served as controls.
All were given standard of care, which included hydroxychloroquine and an antibiotic (or two antibiotics in cases where bacterial infections were diagnosed), plus a steroid in cases involving pulmonary inflammation and/or cytokine storm.4 As reported by the authors:5
“ICU assistance was required by 110 (11.8%) participants. Out of 551 patients treated with calcifediol at admission, 30 (5.4%) required ICU, compared to 80 out of 379 controls (21.1%).
Logistic regression of calcifediol treatment on ICU admission, adjusted by age, gender, linearized 25(OH)D levels at baseline, and comorbidities showed that treated patients had a reduced risk to require ICU (RR 0.18).
Baseline 25(OH)D levels inversely correlated with the risk of ICU admission (RR 0.53). Overall mortality was 10%. In the Intention-to-treat analysis, 36 (6.5%) out of 551 patients treated with calcifediol at admission died compared to 57 patients (15%) out of 379 controls.
Adjusted results showed a reduced mortality for more of 60%. Higher baseline 25(OH)D levels were significantly associated with decreased mortality (RR 0.40).
Age and obesity were also predictors of mortality. Interpretation: In patients hospitalized with COVID-19, calcifediol treatment at the time of hospitalization significantly reduced ICU admission and mortality.”
Renewed Calls for Vitamin D Recommendations
In response to the Spanish findings, British MP David Davis tweeted that “The findings of this large and well conducted study should result in this therapy being administered to every COVID patient in every hospital in the temperate latitudes,” adding that:6
“Since the study demonstrates that the clear relationship between vitamin D and COVID mortality is causal, the U.K. government should increase the dose and availability of free vitamin D to all the vulnerable groups. These approaches will save many thousands of lives. They are overdue and should be started immediately.”
Many others are also calling for official vitamin D recommendations to be issued by their governments. Among them, Emer Higgins,7 a member of the Irish political party Fine Gael, who called on the Irish health minister, Stephen Donnelly, to include vitamin D supplementation in its “Living with COVID-19” strategy, slated for launch at the end of February 2021.
Higgins leaned on evidence from the Irish Covit-D Consortium,8 which shows vitamin D helps optimize your immune response. “There is negligible risk in this strategy and potentially a massive gain,” she said. According to the Covit-D Consortium, the nutrient can lower the risk of death from COVID-19 in the elderly by as much as 700%.9
Low Vitamin D Linked to COVID-19 Outbreaks and Severity
Another recent study10 published in the journal Scientific Reports confirmed vitamin D is a contributing factor to COVID-19 outbreaks and infection severity. According to the authors, the surges in daily positive test results during the fall of 2020 in 18 European countries linearly correlate with latitude, and hence sun exposure and vitamin D levels. They point out that:
“The country surge date corresponds to the time when its sun UV daily dose drops below ≈ 34% of that of 0° latitude. Introducing reported seasonal blood 25-hydroxyvitamin D (25(OH)D) concentration variation into the reported link between acute respiratory tract infection risk and 25(OH)D concentration quantitatively explains the surge dynamics …
The date of the surge is an intrapopulation observation and has the benefit of being triggered only by a parameter globally affecting the population, i.e. decreases in the sun UV daily dose.
The results indicate that a low 25(OH)D concentration is a contributing factor to COVID-19 severity, which, combined with previous studies, provides a convincing set of evidence.”
While it’s well-recognized that most elderly individuals are deficient in vitamin D, the problem is widespread in all age categories, including children.
As noted in a February 2021 study11 comparing vitamin D levels in breast milk collected in 1989 and 2016/2017, vitamin D concentrations are consistently higher during the summer, but overall, vitamin D levels have declined since 1989. As a result, pregnant and lactating mothers and their infants may require vitamin D supplementation for optimal health.
Vitamin D Is Crucial for Optimal T Cell Responses
One of the reasons why vitamin D is so important against COVID-19 has to do with its influence on T cell responses. Animal research12 published in 2014 explained how vitamin D receptor signals regulate T cell responses and therefore play an important role in your body’s defense against viral and bacterial infections.
As noted in that study, when vitamin D signaling is impaired, it significantly impacts the quantity, quality, breadth and location of CD8 T cell immunity, resulting in more severe viral and bacterial infections.
What’s more, according to a December 11, 2020, paper13 in the journal Vaccine: X, high-quality T cell response actually appears to be far more important than antibodies when it comes to providing protective immunity against SARS-CoV-2 specifically:14
“The first SARS-CoV-2 vaccine(s) will likely be licensed based on neutralizing antibodies in Phase 2 trials, but there are significant concerns about using antibody response in coronavirus infections as a sole metric of protective immunity.
Antibody response is often a poor marker of prior coronavirus infection, particularly in mild infections, and is shorter-lived than virus-reactive T-cells …
Strong antibody response correlates with more severe clinical disease while T-cell response is correlated with less severe disease; and antibody-dependent enhancement of pathology and clinical severity has been described.
Indeed, it is unclear whether antibody production is protective or pathogenic in coronavirus infections. Early data with SARS-CoV-2 support these findings. Data from coronavirus infections in animals and humans emphasize the generation of a high-quality T cell response in protective immunity.”
The authors go on to state that epitopes associated with SARS-CoV2 have been identified on CD4 and CD8 T-cells in the blood from patients who have successfully recovered from COVID-19, and that these epitopes “are much less dominated by spike protein than in previous coronavirus infections.”15
As a refresher, aside from SARS-CoV-2, there are six other coronaviruses known to cause respiratory disease in humans:16
- Types 229E, NL63, OC43 and KHU1 are quite common and cause mild to moderate respiratory infections such as the common cold.
- SARS-CoV (Severe Acute Respiratory Syndrome coronavirus), associated with severe respiratory illness.17,18
- MERS-CoV (Middle East Respiratory Syndrome coronavirus) which, like SARS, causes more severe respiratory infections than the four common coronaviruses.19
Understanding the Role of Epitopes
What do they mean by “epitopes associated with SARS-CoV2 have been identified on CD4 and CD8 T-cells”? Epitopes20 are sites on the virus that allow antibodies or cell receptors in your immune system to recognize it. This is why epitopes are also referred to as “antigenic determinants,” as they are the part that is recognized by an antibody, B-cell receptor or T-cell receptor.
Most antigens — substances that bind specifically to an antibody or a T-cell receptor — have several different epitopes, which allow it to be recognized by several different antibodies. Importantly, some epitopes can cause autoimmunological pathogenic priming if you’ve been previously infected with SARS-CoV-2 or exposed via a COVID-19 vaccine.21
In other words, if you’ve had the infection once, and get reinfected (either by SARS-CoV-2 or a sufficiently similar coronavirus), the second bout has the potential to be more severe than the first. Similarly, if you get vaccinated and are then infected with SARS-CoV-2, your infection may be more severe than had you not been vaccinated.
For this reason, “these epitopes should be excluded from vaccines under development to minimize autoimmunity due to risk of pathogenic priming,” a recent paper22 in the Journal of Translational Autoimmunity warns.
One of the reasons why mRNA gene therapy “vaccines” are causing so many problems may in fact be because they have failed to “screen out unsafe epitopes to reduce autoimmunity due to homology between parts of the viral protein and the human proteome,” according to that Journal of Translational Autoimmunity paper.23
Natural SARS-CoV-2 Infection Induces Broad Epitope Coverage
The authors of the Vaccine: X paper point out that while most COVID-19 gene therapy “vaccines” focus on the SARS-CoV-2 spike protein as a natural antigen, “natural infection by SARS-CoV-2 induces broad epitope coverage, cross-reactive with other betacoronviruses.”
Indeed, this has been demonstrated in a number of studies, including a Singaporean study24,25,26 that found common colds caused by the betacoronaviruses OC43 and HKU1 might make you more resistant to SARS-CoV-2 infection, and that the resulting immunity might last as long as 17 years.
In other words, if you’ve beat a common cold caused by a OC43 or HKU1 betacoronavirus in the past, you may have a 50/50 chance of having defensive T-cells that can recognize and help defend against SARS-CoV-2. What the Vaccine: X authors are basically warning about is that the so-called vaccines are unlikely to provide the same level of immunity as natural infection does, and may even cause pathogenic priming.
Vitamin D Speeds Viral Clearance
Other research,27 published in November 2020 in the Postgraduate Medical Journal, shows oral vitamin D supplementation also helps speed up SARS-CoV-2 viral clearance. This study included only asymptomatic or mildly symptomatic SARS-CoV-2-positive individuals who also had vitamin D deficiency (a vitamin D blood level below 20 ng/mL).
Participants were randomly assigned to receive either 60,000 IUs of oral cholecalciferol (nano-liquid droplets) or a placebo for seven days. The target blood level was 50 ng/mL. Anyone who had not achieved a blood level of 50 ng/mL after the first seven days continued to receive the supplement until they reached the target level.
Periodically, all participants were tested for SARS-CoV-2 as well as fibrinogen, D-dimer, procalcitonin and CRP, all of which are inflammatory markers. The primary outcome measure of the study was the proportion of patients testing negative for COVID-19 before Day 21 of the study, as well as changes in inflammatory markers. As reported by the authors:28
“Forty SARS-CoV-2 RNA positive individuals were randomized to intervention (n=16) or control (n=24) group. Baseline serum 25(OH)D was 8.6 and 9.54 ng/mL, in the intervention and control group, respectively.
10 out of 16 patients could achieve 25(OH)D>50 ng/ml by day-7 and another two by day-14 … 10 (62.5%) participants in the intervention group and 5 (20.8%) participants in the control arm became SARS-CoV-2 RNA negative. Fibrinogen levels significantly decreased with cholecalciferol supplementation unlike other inflammatory biomarkers.
[A] greater proportion of vitamin D-deficient individuals with SARS-CoV-2 infection turned SARS-CoV-2 RNA negative with a significant decrease in fibrinogen on high-dose cholecalciferol supplementation.”
More Evidence Vitamin D Impacts COVID-19
If you haven’t already gone to the free website I created to educate the world about vitamin D, please do now. It’s www.stopcovidcold.com. You can download the free condensed version of the paper I had published last year that is easier to read and full of graphics to illustrate the information.
October 31, 2020, my own vitamin D review,29 co-written with William Grant, Ph.D., and Dr. Carol Wagner, both of whom are part of the GrassrootsHealth expert vitamin D panel, was published in the peer-reviewed journal Nutrients. You can read the paper for free on the journal’s website.
As noted in that paper, dark skin color, increased age, pre-existing chronic conditions and vitamin D deficiency are all features of severe COVID disease, and of these, vitamin D deficiency is the only factor that is readily and easily modifiable.
You may be able to reverse chronic disease, but that typically takes time. Optimizing your vitamin D, on the other hand, can be achieved in just a few weeks, thereby significantly lowering your risk of severe COVID-19.
In our paper, we review several of the mechanisms by which vitamin D can reduce your risk of COVID-19 and other respiratory infections, including but not limited to the following:30
- Reducing the survival and replication of viruses31
- Reducing inflammatory cytokine production
- Maintaining endothelial integrity — Endothelial dysfunction contributes to vascular inflammation and impaired blood clotting, two hallmarks of severe COVID-19
- Increasing angiotensin-converting enzyme 2 (ACE2) concentrations, which prevents the virus from entering cells via the ACE2 receptor — ACE2 is downregulated by SARS-CoV-2 infection, and by increasing ACE2, you also avoid excessive accumulation of angiotensin II, a peptide hormone known to increase the severity of COVID-19
Vitamin D is also an important component of COVID-19 prevention and treatment for the fact that it:
- Boosts your overall immune function by modulating your innate and adaptive immune responses
- Reduces respiratory distress32
- Improves overall lung function
- Helps produce surfactants in your lungs that aid in fluid clearance33
- Lowers your risk of comorbidities associated with poor COVID-19 prognosis, including obesity,34 Type 2 diabetes,35 high blood pressure36 and heart disease37
Data from 14 observational studies — summarized in Table 1 of our paper38 — suggest that vitamin D blood levels are inversely correlated with the incidence and/or severity of COVID-19, and the evidence currently available generally satisfies Hill’s criteria for causality in a biological system.39 Our paper40 also details several features of COVID-19 that suggest vitamin D deficiency is at play in this illness.
How to Optimize Your Vitamin D
While most people would probably benefit from a vitamin D3 supplement, it’s important to get your vitamin D level tested before you start supplementing. The reason for this is because you cannot rely on blanket dosing recommendations. The crucial factor here is your blood level, not the dose, as the dose you need is dependent on several individual factors, including your baseline blood level.
Data from GrassrootsHealth’s D*Action studies suggest the optimal level for health and disease prevention is between 60 ng/mL and 80 ng/mL, while the cutoff for sufficiency appears to be around 40 ng/mL. In Europe, the measurements you’re looking for are 150 to 200 nmol/L and 100 nmol/L respectively.
I’ve published a comprehensive vitamin D report in which I detail vitamin D’s mechanisms of action and how to ensure optimal levels. I recommend downloading and sharing that report with everyone you know. A quick summary of the key steps is as follows:
1. First, measure your vitamin D level — One of the easiest and most cost-effective ways of measuring your vitamin D level is to participate in the GrassrootsHealth’s personalized nutrition project, which includes a vitamin D testing kit.
Once you know what your blood level is, you can assess the dose needed to maintain or improve your level. If you cannot get enough vitamin D from the sun (you can use the DMinder app41 to see how much vitamin D your body can make depending on your location and other individual factors), then you’ll need an oral supplement.
2. Assess your individualized vitamin D dosage — To do that, you can either use the chart below, or use GrassrootsHealth’s Vitamin D*calculator. To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5. To calculate how much vitamin D you may be getting from regular sun exposure in addition to your supplemental intake, use the DMinder app.42
3. Retest in three to six months — Lastly, you’ll need to remeasure your vitamin D level in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you.
Take Your Vitamin D With Magnesium and K2
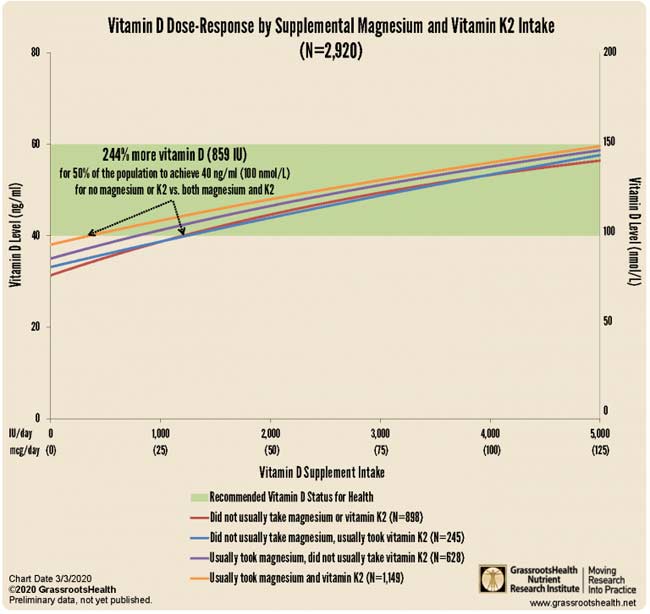
As detailed in “Magnesium and K2 Optimize Your Vitamin D Supplementation,” it’s strongly recommended to take magnesium and K2 concomitant with oral vitamin D. Data from nearly 3,000 individuals reveal you need 244% more oral vitamin D if you’re not also taking magnesium and vitamin K2.43
What this means in practical terms is that if you take all three supplements in combination, you need far less oral vitamin D in order to achieve a healthy vitamin D level.