The White House said on Tuesday that weekly shipments of coronavirus vaccines to the states would rise by one million doses to 14.5 million, as vaccine manufacturers continue to ramp up production.
The figure was provided to governors in a call with Jeffrey Zeints, the president’s coronavirus response coordinator, said Jen Psaki, the White House press secretary, on Tuesday. With tens of millions of eligible Americans waiting to get shots, state officials have been clamoring for more vaccine, saying health practitioners could easily double or triple the number of shots they are administering.
Ms. Psaki said the increase was the fifth boost in distribution in five weeks, and said it came just short of doubling the vaccine shipments underway at the time Mr. Biden took office on Jan. 20.
Before snowstorms disrupted vaccine distribution last week, the average number of daily doses administered across the country had been steadily increasing as the two federally approved vaccine manufacturers, Pfizer and Moderna, get more efficient and expand production. While that acceleration was expected well before Mr. Biden assumed office, officials have been anxious to highlight every increase in shipments as evidence that the new administration is fiercely battling the pandemic. As of Tuesday, the seven-day average rate of doses administered across the country was 1.4 million a day, after peaking at about 1.7 million before the storms, according to a New York Times vaccine database.
Many vaccination appointments last week that were postponed by snowstorms and other disruptive weather are resuming this week. In Los Angeles, Mayor Eric Garcetti said vaccinations would start back up again on Tuesday at all of the city-run sites and indicated that people whose inoculations had been delayed by the weather would be given priority over those making new appointments.
At a congressional hearing Tuesday morning, top officials from Pfizer and Moderna reiterated previous supply commitments in front of lawmakers Both firms promised earlier this month to deliver a total of 400 million doses by the end of May, weeks ahead of schedule, and a total of 600 million by the end of July.
John Young, Pfizer’s chief business officer, testified that his firm will be able to ship more than 13 million doses per week by mid-March, compared to a weekly shipment of just four to five million at the start of this month. He cited a variety of reasons, including federal regulatory approval to count each vial as holding six doses instead of five, more efficient production processes and faster laboratory tests of the vaccine before it is shipped.
Dr. Stephen Hoge, president of Moderna, testified that his company expects to double its current shipments to more than 10 million per week by April.
More supply is expected to come from Johnson & Johnson, but not as quickly as federal officials initially had hoped. Federal regulators are widely expected to grant emergency use authorization for that vaccine by early next week.
Dr. Richard Nettles, a company vice president testified that the firm is prepared to deliver 20 million doses of its vaccine by the end of March. Of that, he said, nearly four million doses could be shipped as soon as the Food and Drug Administration gives the firm the green light. Unlike the other two authorized vaccines, Johnson & Johnson’s requires only one dose.
Dr. Nettles’s testimony was the first public indication by the company of how many doses it could supply before April.
His promise falls short of the 37 million doses that Johnson & Johnson’s federal contract called for it to deliver by the end of March. Asked what accounted for the gap, Dr. Nettles did not directly answer. But he implied that the company would catch up, saying the firm will deliver the entire 100 million doses it has promised by the end of June, as the contract requires.
Together with the deliveries from Moderna and Pfizer, which developed its vaccine with a German partner, BioNTech, the new supply from Johnson & Johnson would mean that the nation would have enough doses on hand by the end of next month to vaccinate about 130 million Americans. That would cover roughly half of all eligible adults and 40 percent of the total population.
Nicholas Bogel-Burroughs contributed reporting.

A variant first discovered in California in December is more contagious than earlier forms of the coronavirus, two new studies have shown, fueling concerns that emerging mutants like this one could hamper the sharp decline in cases over all in the state and perhaps elsewhere.
In one of the new studies, researchers found that the variant has spread rapidly in a San Francisco neighborhood in the past couple of months. The other report confirmed that the variant has surged across the state, and revealed that it produces twice as many viral particles inside a person’s body as other variants do. That study also hinted that the variant may be better than others at evading the immune system — and vaccines.
“I wish I had better news to give you — that this variant is not significant at all,” said Dr. Charles Chiu, a virologist at the University of California, San Francisco. “But unfortunately, we just follow the science.”
Neither study has yet been published in a scientific journal. And experts don’t know how much of a public health threat this variant poses compared with others that are also spreading in California.
A variant called B.1.1.7 arrived in the United States from Britain, where it swiftly became the dominant form of the virus and overloaded hospitals there. Studies of British medical records suggest that B.1.1.7 is not only more transmissible, but more lethal than earlier variants.
Some experts said the new variant in California was concerning, but unlikely to create as much of a burden as B.1.1.7.
“I’m increasingly convinced that this one is transmitting more than others locally,” said William Hanage, an epidemiologist at the Harvard T.H. Chan School of Public Health who was not involved in the research. “But there’s not evidence to suggest that it’s in the same ballpark as B.1.1.7.”
Dr. Chiu first stumbled across the new variant by accident. In December, he and other researchers in California were worried about the discovery of B.1.1.7 in Britain. They began looking through their samples from positive coronavirus tests in California, sequencing viral genomes to see if B.1.1.7 had arrived in their state.
On New Year’s Eve, Dr. Chiu was shocked to find a previously unknown variant that made up one-quarter of the samples he and his colleagues had collected. “I thought that was crazy,” he said.
It turned out that researchers at the Cedars-Sinai Medical Center in Los Angeles separately discovered the same variant surging to high levels in Southern California. Dr. Chiu announced his initial finding, and the Cedars-Sinai team went public two days later.
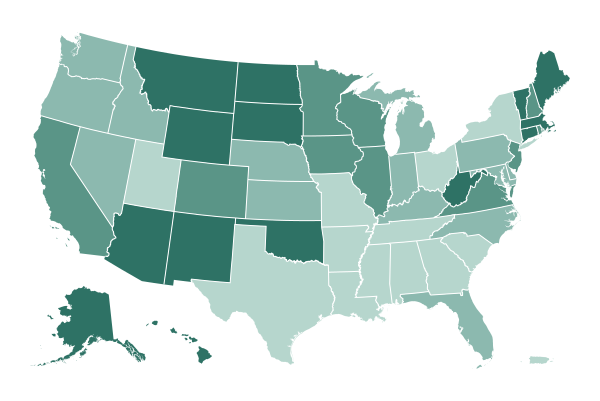
Since then, researchers have been looking more closely at the new variant, known as B.1.427/B.1.429, to pinpoint its origin and track its spread. It has shown up in 45 states to date, and in several other countries, including Australia, Denmark, Mexico and Taiwan. But it has so far taken off only in California.
It was unclear at first whether the variant was inherently more transmissible than others, or whether it had surged in California because of gatherings that became superspreading events.

Federal regulators have informed Pfizer and BioNTech that they plan to approve the companies’ request to store their vaccine at standard freezer temperatures instead of in ultra-cold conditions, potentially expanding the number of sites that could administer shots, according to two people familiar with the companies who spoke on condition of anonymity.
The Food and Drug Administration is expected to announce new guidance to providers as early as Tuesday, modifying documents related to the emergency use authorization that was previously granted for the vaccine, they said.
Pfizer and BioNTech, its German partner, said Friday that they had submitted new data to the F.D.A. showing their vaccine could be safely stored at -13 to 5 degrees Fahrenheit for up to two weeks. That could open up the possibility that smaller pharmacies and doctors’ offices could administer shots using their existing refrigerators or freezers.
Regulators had previously approved distribution only if the vaccine was stored in freezers that kept it between -112 and -76 degrees Fahrenheit. Pfizer ships its vials in specially designed containers that can be used as temporary storage for up to 30 days, then refilled with dry ice every five days. The vaccine can be refrigerated for up to five days in a standard refrigerator if it had not yet been diluted for use in patients.

New coronavirus cases and hospitalizations are on the downswing in the United States and around the world, but hot spots along the East Coast have been sticking around longer compared to the rest of the country.
In the current wave of regional outbreaks, eight states that border the Atlantic Ocean have seen upticks in the past few months and only recently have started to level off or decline.
South Carolina leads the nation with the highest rate of new virus cases, followed by New York, New Jersey, Rhode Island, North Carolina, Florida, Delaware and Georgia.
It has become a familiar pattern across the country — cases go up in one region, and down in another — a sequence driven in some part by weather. A few months ago, the Upper Midwest, where it starts to get cold in the fall, was outpacing other regions in new infections. And before that, cases in the Sunbelt surged.
“It’s whack-a-mole,” said Leana Wen, an emergency physician and public health professor at George Washington University. “One part of the country sees a surge, and then another, and then it declines.”
In New York City on Tuesday, Mayor Bill de Blasio said that he believed the city’s case numbers and positive test rates had not declined more dramatically because of population density, a legacy of poverty and a high number of New Yorkers without health care.
“There’s challenges for sure,” Mr. de Blasio said at a news conference. “But I feel very good about our ability to turn it around with intensive vaccination — if we can get supply.”
According to health data, the city’s seven-day average positive test rate was 7.3 percent on Sunday, the latest day for which data was available, down from a recent peak of 9.7 percent from Jan. 2-4. (New York State, which compiles testing data and calculates statistics differently from the city, most recently reported the city’s seven-day average at 4.49 percent, down from 6.4 percent on Jan. 4-7.)
New cases have declined to half their peak globally, largely because of steady improvements in some of the same places that endured devastating outbreaks this winter. The global decline has been driven by six countries, led by the United States, which still leads the world in the number of new cases a day, based on a seven-day average, followed by Brazil and France.
Public health experts in the worst-hit countries attribute the progress to some combination of increased adherence to social distancing and mask wearing, the seasonality of the virus and a buildup of natural immunity among groups with high rates of existing infection.
“It’s a great moment of optimism, but it’s also very fragile in a lot of ways,” said Wafaa El-Sadr, an epidemiologist at Columbia University’s Mailman School of Public Health. “We see the light at the end of the tunnel, but it’s still a long tunnel.”
The emergence of new variants of the virus, however, has caused great concern, increasing the pressure to get people vaccinated as soon as possible. A variant first found in Britain is spreading rapidly in the United States, and it has been implicated in surges in Ireland, Portugal and Jordan. The variant first found in South Africa, which weakens the effectiveness of vaccines, has also surfaced in the United States.
Allison McCann, Lauren Leatherby and Josh Holder contributed reporting.

BEIRUT, Lebanon — The Covid-19 vaccination drive in Lebanon erupted in scandal on Tuesday when 16 lawmakers received shots inside the parliament building, violating regulations aimed at keeping the process fair and transparent.
The vaccination program, financed by $34 million from the World Bank, began earlier this month when the country received its first doses. To try to ensure accountability in a country known for corner-cutting and corruption, the government is requiring citizens to register for vaccination through an online portal. Medical workers and people over 75 are supposed to get the shots first, administered in official vaccination centers.
On Tuesday, Adnan Daher, the parliamentary secretary, confirmed to reporters that 16 lawmakers had received shots. He said the lawmakers were all of the proper age and their turn to be vaccinated had come. But according to lists compiled by local news outlets, about half were younger than 75.
Elie Ferzli, a lawmaker in his early 70s who got the shot on Tuesday, denied in a telephone interview that he had jumped the line, and said he was “shocked” by the public outrage over the shots.
“I have meetings every day in the parliament, so how am I supposed to keep doing my job normally and helping people?” he said.
Officials overseeing the vaccination program, though, cried foul.
Dr. Abdul Rahman Bizri, the head of Lebanon’s vaccine committee, threatened to resign over what he condemned as “a violation we cannot stay silent about,” but he decided to stay on.
Saroj Kumar Jha, the World Bank’s director for the region that includes Lebanon, wrote on Twitter before the reports were confirmed that letting lawmakers jump the line was “not in line with the national plan,” and added, “Everyone has to register and wait for their turn!”
He said that if the rules were broken, the World Bank could suspend its support for the vaccination program and Lebanon’s Covid-19 response generally.
A World Bank spokeswoman did not respond to a query on Tuesday about how the bank would handle the incident.
Hwaida Saad contributed reporting.

Scotland will emerge from its lockdown in three-week stages over the next few months, beginning with reopening schools, First Minister Nicola Sturgeon announced on Tuesday.
Scotland’s schools, which began reopening on Monday, will resume in-person instruction in phases through March, Ms. Sturgeon said, and stay-at-home orders would begin to be relaxed on April 5, allowing communal worship and some businesses to reopen. Most businesses and activities would be allowed to resume after April 26, Ms. Sturgeon said.
About one-third of adults in Scotland have received at least the first dose of a Covid vaccine. The progress with vaccinations and the early data suggesting that vaccination significantly reduces the risk of hospitalization were “extremely welcome and encouraging news,” Ms. Sturgeon told lawmakers on Tuesday.
She said the timeline for relaxing restrictions would be contingent on data showing that the virus was being kept at bay. To that end, she said, contact tracing was vital, and travel restrictions would probably remain in force for some time. “Maximum suppression is important for our chances of getting back to normal,” she said.
“I know how hard all of this continues to be after 11 long months of this pandemic,” Ms. Sturgeon said, but “I think that we can be much more hopeful today than we have been able to be this entire pandemic.”
On Monday, Prime Minister Boris Johnson laid out a long-awaited plan for completely lifting restrictions in England by June 21. His plan also begins with schools, and would keep pubs and most other businesses shut for at least another month.
Ms. Sturgeon’s plan for Scotland is more limited in scope, at least so far; she said more details would be released in March.
Much of Scotland has been locked down since early January because of the rapid spread of a new variant of the virus. The variant now accounts for more than 85 percent of new cases in Scotland, Ms. Sturgeon said on Tuesday. The country reported 655 new cases on Monday and 56 deaths from Covid-19.
The first studies of Britain’s mass inoculation program indicate that a single dose of either the Oxford-AstraZeneca or Pfizer-BioNTech vaccine averts most coronavirus-related hospitalizations, researchers said on Monday, though they said it was too early to give precise estimates of the effect. Scotland is aiming to offer every adult a first dose of vaccine by the end of July.

State lawmakers across the country, most of them Republicans, are moving aggressively to strip the powers of governors, often Democrats, who have taken on extraordinary authority to limit the spread of the coronavirus for nearly a year.
In a kind of rear-guard action, legislatures in more than 30 states are trying to restrict the power of governors to act unilaterally under extended emergencies that have traditionally been declared in brief bursts after floods, tornadoes or similar disasters. Republicans are seeking to harness the widespread fatigue of many Americans toward closed schools, limits on gatherings and mask mandates as a political cudgel to wield against Democrats.
Lawmakers frame the issue as one of checks and balances, arguing that governors gained too much authority over too many aspects of people’s lives. These legislators are demanding a say in how long an emergency can last, and insisting that they be consulted on far-reaching orders like closing schools and businesses.
But governors respond that a pandemic cannot be fought by committee. They say that the same Republicans who politicized the science of the pandemic last year, following former President Donald J. Trump in waging a new battle in the culture wars, should not be trusted with public health.
Last April, when governors in all 50 states declared disaster emergencies for the first time in the country’s history, support for their initial stay-at-home orders to slow the virus’s spread was generally bipartisan.
But that soon evaporated as Mr. Trump, obsessed about the economy in an election year, played down the virus. Supporters echoed his dismissal of health experts and defied governors who filled the federal leadership vacuum to manage the pandemic — especially Democratic governors whom the president took to insulting, issuing cries to “liberate” states like Michigan.
Across the country, lawmakers in 37 states have introduced more than 200 bills or resolutions this year to clip the emergency powers of governors, according to the lobbying firm Stateside, which focuses on state governments.

The enormous scale of illness and death wrought by the coronavirus is traced in figures that have grown so far beyond the familiar yardsticks of daily life that they can sometimes be difficult to get a handle on.
The news on Monday that the United States had recorded 500,000 Covid-19-related deaths in just a year is just the latest example.
One way to put that in context is to compare it to other major causes of death in 2019, the year before the pandemic took hold in the country.
500,000 deaths is …
-
Three times the number of people who died in the U.S. in any kind of accident, including highway accidents, in 2019 (167,127).
-
More than eight times the number of deaths from influenza and pneumonia (59,120).
-
More than 10 times the number of suicides (48,344).
-
More than the number of deaths from strokes, diabetes, kidney disease, Alzheimer’s and related causes, combined (406,161).
-
Only heart disease (655,381) and cancer (599,274) caused more deaths.
When full data for 2020 is available from the Centers for Disease Control and Prevention, Covid-19 will certainly be one of the leading killers. But trying to project where it will rank may be complicated. A very large share of deaths from Covid-19 have been people who were medically vulnerable because of other significant health problems like cancer, lung or heart disease. Some number of them would probably have succumbed to those causes, and been counted in those categories, if their deaths had not been hastened by Covid-19.

President Biden’s nominee for health secretary, Xavier Becerra, pledged Tuesday morning to work to “restore faith in public health institutions” and to “look to find common cause” with his critics, as Republicans sought to paint him as a liberal extremist who is unqualified for the job.
Appearing before the Senate Committee on Health, Education, Labor and Pensions, Mr. Becerra, the attorney general of California, was grilled by Republicans who complained that he has no background in the health profession, and who targeted his support for the Affordable Care Act and for abortion rights.
“Basically, you’ve been against pro-life, on the record,” Senator Mike Braun, Republican of Indiana, said to Mr. Becerra. He asked whether Mr. Becerra would commit to not using taxpayer money for abortions, which is currently barred by federal law, except in instances where the life of the mother is at stake, or in incest or rape.
“I will commit to following the law,” Mr. Becerra replied — leaving himself some wiggle room should the law change.
Tuesday’s appearance was the first of two Senate confirmation hearings for Mr. Becerra; he is scheduled to appear before the Senate Finance Committee on Wednesday. Despite the tough questions, Mr. Becerra appears headed for confirmation in a Senate evenly split between Democrats and Republicans, but with Vice President Kamala Harris available to break a tie.
If confirmed, Mr. Becerra will immediately face a daunting task in leading the department at a critical moment, during a pandemic that has claimed half a million lives and has taken a particularly devastating toll on people of color. He would be the first Latino to serve as secretary of the federal Department of Health and Human Services.
While Mr. Becerra, a former member of Congress, lacks direct experience as a health professional, he took a deep interest in health policy while in Washington and helped write the Affordable Care Act. He has more recently been at the forefront of legal efforts to defend it, leading 20 states and the District of Columbia in a campaign to protect the act from being dismantled by Republicans.
Republicans and their allies in the conservative and anti-abortion movements have seized on Mr. Becerra’s defense of the A.C.A. as well as his support for abortion rights.
The Conservative Action Project, an advocacy group, issued a statement on Monday signed by dozens of conservative leaders, including several former members of Congress, complaining that Mr. Becerra had a “troubling record” with respect to “policies relating to the sanctity of life, human dignity and religious liberty.”
They cited in particular his vote against banning “late-term abortion,” and accused him of using his role as attorney general “to tip the scales in favor of Planned Parenthood,” a group that advocates abortion rights. Asked by Senator Mitt Romney, Republican of Utah, about the late-term abortion vote, Mr. Becerra noted that his wife is an obstetrician-gynecologist, and said he would “work to find common ground” on the issue. Mr. Romney was not impressed. “It sounds like we’re not going to reach common ground there,” he replied.
Democrats are emphasizing Mr. Becerra’s experience leading one of the nation’s largest justice departments through an especially trying period, and his up-from-the-bootstraps biography. A son of immigrants from Mexico, he attended Stanford University as an undergraduate and for law school. He served 12 terms in Congress, representing Los Angeles, before becoming the attorney general of his home state in 2017.

The world needs monkeys, whose DNA closely resembles that of humans, to develop Covid-19 vaccines. But a global shortage, resulting from the unexpected demand caused by the pandemic, has been exacerbated by a recent ban on the sale of wildlife from China, the leading supplier of the lab animals.
The latest shortage has revived talk about creating a strategic monkey reserve in the United States, an emergency stockpile similar to those maintained by the government for oil and grain.
As new variants of the coronavirus threaten to make the current batch of vaccines obsolete, scientists are racing to find new sources of monkeys, and the United States is reassessing its reliance on China, a rival with its own biotech ambitions.
The pandemic has underscored how much China controls the supply of lifesaving goods, including masks and drugs, that the United States needs in a crisis.
American scientists have searched private and government-funded facilities in Southeast Asia as well as Mauritius, a tiny island nation off southeast Africa, for stocks of their preferred test subjects, rhesus macaques and cynomolgus macaques, also known as long-tailed macaques.
But no country can make up for what China previously supplied. Before the pandemic, China provided over 60 percent of the 33,818 primates, mostly cynomolgus macaques, imported into the United States in 2019, according to analyst estimates based on data from the Centers for Disease Control and Prevention.
The United States has about 22,000 lab monkeys — predominantly pink-faced rhesus macaques — at its seven primate centers. About 600 to 800 of those animals have been subject to coronavirus research since the pandemic began.
Scientists say monkeys are the ideal specimens for researching coronavirus vaccines before they are tested on humans. The primates share more than 90 percent of our DNA, and their similar biology means they can be tested with nasal swabs and have their lungs scanned. Scientists say it is almost impossible to find a substitute to test Covid-19 vaccines in, although drugs such as dexamethasone, the steroid that was used to treat former President Donald J. Trump, have been tested in hamsters.
The United States once relied on India to supply rhesus macaques. But in 1978, India halted its exports after Indian news outlets reported that the monkeys were being used in military testing in the United States. Pharmaceutical companies searched for an alternative, and eventually landed on China.
But the pandemic upset what had been a decades-long relationship between American scientists and Chinese suppliers.

Over the past year, hospital intensive care units have been overrun with critically ill Covid-19 patients, who develop severe pneumonia and other organ dysfunction. At times, the influx of coronavirus cases overwhelmed the resources in the units and the complexity of the care these patients required.
An interactive graphic by The New York Times explores how coronavirus surges affected I.C.U.s and their specialty medical staff.
New cases in the United States have fallen since their peak in early January, but almost three-quarters of the nation’s I.C.U. beds were occupied over the week ending Feb. 18.
The national average for adult I.C.U. occupancy was 67 percent in 2010, according to the Society of Critical Care Medicine, though this number and all hospitalization figures vary depending on the place, time of year and size of hospital.
When the coronavirus rips through a community, I.C.U.s fill up. Hospitals have been forced to improvise, expanding capacity by creating I.C.U.s in areas normally used for other purposes, like cardiac or neurological care, and even hallways or spare rooms.
Elective surgeries often get put on hold to keep beds available, and early in the pandemic, hospitals saw huge drops in people admitted for any reason other than Covid-19. I.C.U. staff members, regardless of specialty, often spent most or all of their time on Covid patients.
“We’re all exhausted,” said Dr. Nida Qadir, the co-director of the medical intensive care unit at Ronald Reagan UCLA Medical Center. “We’ve had to flex up quite a bit.”

On Sunday afternoon, several hundred people gathered in the small town of Codogno, about 35 miles south of Milan.
The group, including local dignitaries, army veterans and hospital workers, was meeting for the unveiling of a small garden, featuring a quince tree and a sculpture with three steel columns. Inscribed on a platform below the columns were the words “Resilience,” “Community” and “Restart.”
The garden is one of Italy’s first memorials to those who have died after contracting the coronavirus, and it was dedicated on the anniversary of the day news broke that a 38-year-old resident of Codogno, who became known as Patient One, had the virus. That man was Italy’s first known case of local transmission. The next day, the police sealed the town, and no one could enter or leave.
“It was horrific, absurd and unimaginable that this nightmare could unfold in Codogno,” Francesco Passerini, the town’s mayor and the driving force behind the memorial, said in a telephone interview before the ceremony. “Nearly everyone has lost someone,” he added.
For some, it may seem too early to create a memorial to a pandemic that is still raging. More than 200 people were reported to have died from Covid-19 in Italy on Sunday, and the country is in a state of emergency until at least the end of April, with strict travel restrictions in place.
But the memorial in Codogno and others planned elsewhere in Europe are not intended as sweeping monuments to the historical moment, but simple places to grieve and reflect.
GLOBAL ROUNDUP

While the pandemic has been difficult for many in Japan, the pressures have been compounded for women. As in many countries, more women have lost their jobs. In Tokyo, the country’s largest metropolis, about one in five women live alone, and the exhortations to stay home and avoid visiting relatives have exacerbated feelings of isolation.
Other women have struggled with the deep disparities in the division of housework and child care during the work-from-home era, or suffered from increases in domestic violence and sexual assault.
The rising psychological and physical toll of the pandemic has been accompanied by a worrisome spike in suicide among women. In Japan, 6,976 women died by suicide last year, nearly 15 percent more than in 2019. It was the first year-over-year increase in more than a decade.
Each suicide — and suicide attempt — represents an individual tragedy rooted in a complex constellation of reasons. But the increase among women, which extended across seven straight months last year, has concerned government officials and mental health experts who have worked to reduce what had been among the highest rates of suicide in the world. (While more men than women died by suicide last year, fewer men did so than in 2019. Over all, suicides increased slightly less than 4 percent.)
The situation has reinforced longstanding challenges for Japan. Talking about mental health issues, or seeking help, is still difficult in a society that emphasizes stoicism.
The pandemic has also amplified the stresses in a culture that is grounded in social cohesion and relies on peer pressure to drive compliance with government requests to wear masks and practice good hygiene. Women, who are often designated as primary caregivers, at times fear public humiliation if they somehow fail to uphold these measures or get infected with the coronavirus.
In one widely publicized account, a 30-something woman who had been recuperating from the coronavirus at home died by suicide. The Japanese news media seized on her note expressing anguish over the possibility that she had infected others and caused them trouble, while experts questioned whether shame may have driven her to despair.
-
Galicia, in northwestern Spain, on Tuesday became the first region of Spain to approve a law that imposes fines on people who refuse to get vaccinated against Covid-19. The law, which was approved in Galicia’s regional parliament, sets fines of as much as 60,000 euros, or nearly $73,000, if a person’s decision to refuse vaccination is deemed to result in “a very serious risk or harm for the health of the population.” The law was approved by lawmakers of the conservative Popular Party, which governs Galicia, but fiercely criticized by opposition politicians as an attack on individual choice. The central government of Spain, which is led by the Socialist Party, also opposed the Galician law.
-
Ukraine said it had obtained its first vaccine supply on Tuesday, buying 500,000 doses of an Oxford-AstraZeneca version made in India. Ukraine, which has been reporting more than 5,000 cases a day, said the doses were earmarked for front-line medical workers. “We are grateful to our Indian partners,” President Volodymyr Zelensky of Ukraine wrote on Twitter after the delivery on Tuesday.
-
Two European soccer giants, Atlético Madrid and Chelsea, will meet in the Champions League on Tuesday — in Bucharest, Romania. On Wednesday, Manchester City will play the German team Borussia Mönchengladbach — in Budapest, the Hungarian capital, where the English champion Liverpool beat Germany’s RB Leipzig last week. In the Europa League, the continent’s second-tier club championship, neutral sites are now almost as common as home games. The pandemic has wreaked havoc with international sports schedules for a year, and that chaos continues to affect soccer’s biggest club tournaments. The reasons — government edicts, travel restrictions and quarantine rules — vary around Europe. UEFA, the European soccer governing body that runs the competitions, has decided that if restrictions adversely affect any game, it will be played at a neutral site where travel is permitted. But the decision to play knockout games in places seemingly chosen at random has led to confusion, and not a little grumbling
Raphael Minder, Andrew E. Kramer and Victor Mather contributed reporting.