A previous version of this story incorrectly reported the percentage of health-care workers in the survey who said their mental health was negatively impacted by worry or stress related to covid-19. The correct result is 62 percent, not 61 percent. The story has been corrected.
Worry, exhaustion, constantly changing safety rules and long hours of wearing PPE are just a few things America’s health-care workers cite as the hardest parts of going to work on the front lines of the coronavirus pandemic.
Their work has saved countless lives but also taken a personal toll: 62 percent say worry or stress related to covid-19 has had a negative effect on their mental health. A 55 percent majority feel “burned out” going to work. Nearly half of all health-care workers say worry or stress has caused them to have trouble sleeping or to sleep too much.
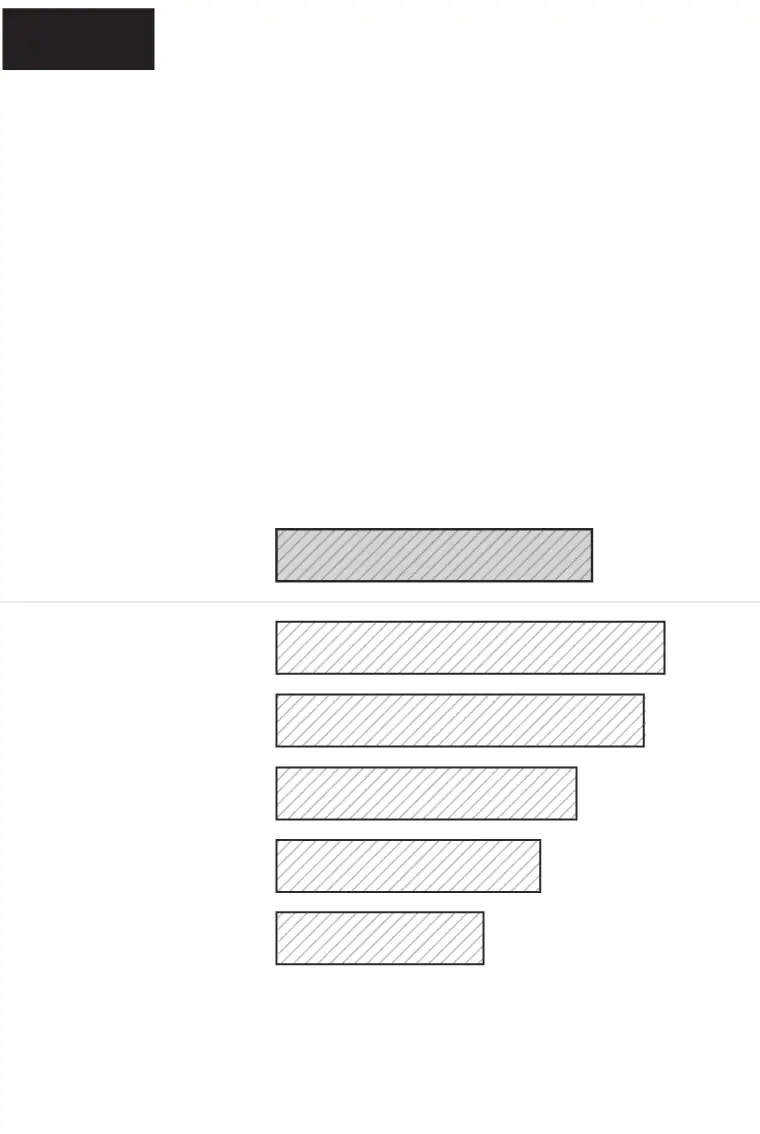
Washington Post-Kaiser
Family Foundation poll
6 in 10 health-care workers say their mental health suffered from coronavirus worry
Q: Do you feel that worry or stress related to covid-19 has had a negative impact on your mental health, or not?
Percent saying covid-19 has had a
negative impact on mental health
Health-care
workers
overall
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3.5 percentage points. Error margins higher among subgroups.
Washington Post-Kaiser Family
Foundation poll
6 in 10 health-care workers say their mental health suffered from coronavirus worry
Q: Do you feel that worry or stress related to covid-19 has had a negative impact on your mental health, or not?
Percent saying covid-19 has had a
negative impact on mental health
Health-care
workers overall
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3.5 percentage points. Error margins higher among subgroups.
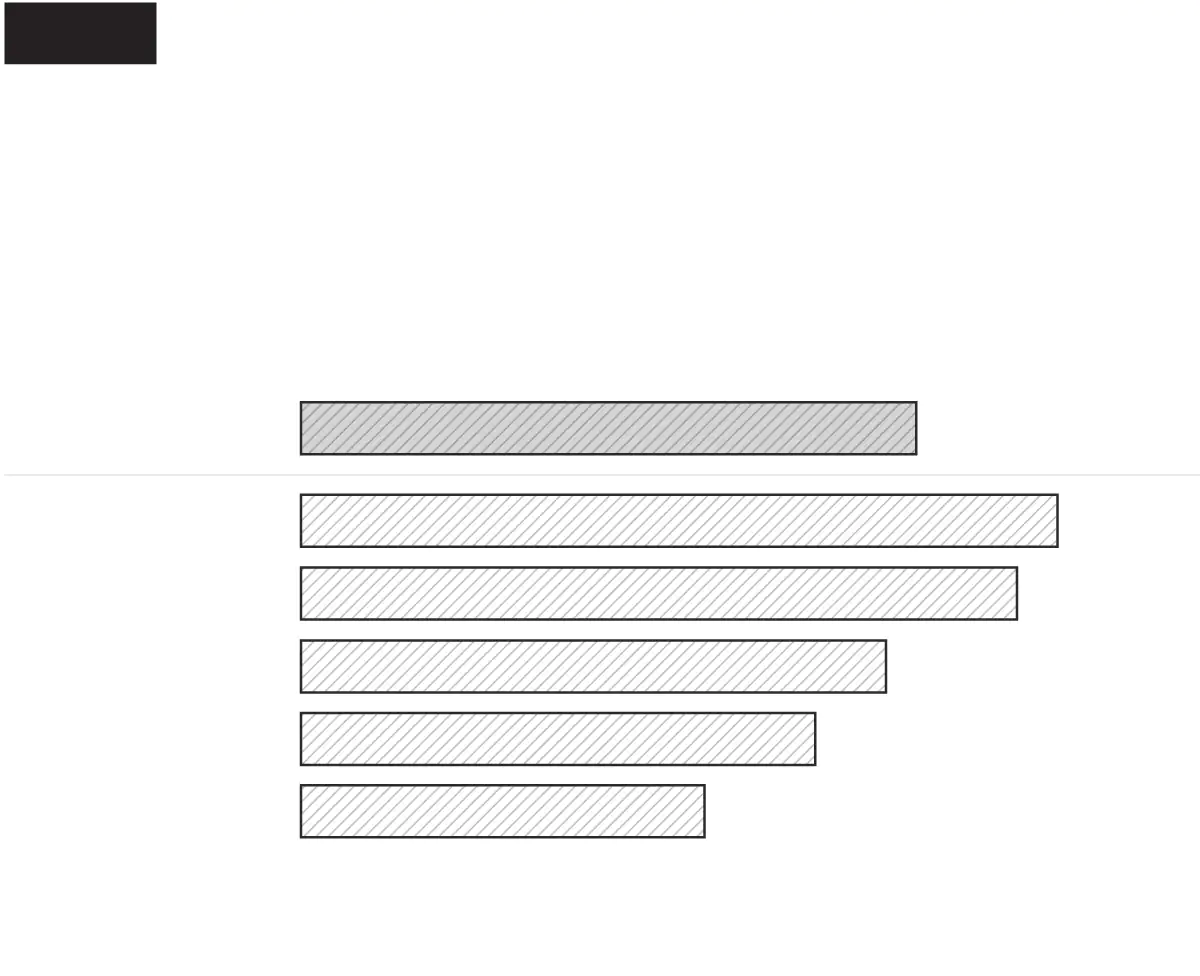
Washington Post-Kaiser Family Foundation poll
6 in 10 health-care workers say their mental health suffered from coronavirus worry
Q: Do you feel that worry or stress related to covid-19 has had a negative impact on your mental health, or not?
Percent saying covid-19 has had a negative impact
on mental health
Health-care
workers overall
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3.5 percentage points. Error margins higher among subgroups.
Washington Post-Kaiser Family Foundation poll
6 in 10 health-care workers say their mental health suffered from coronavirus worry
Q: Do you feel that worry or stress related to covid-19 has had a negative impact on your mental health, or not?
Percent saying covid-19 has had a negative impact
on mental health
Health-care
workers overall
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3.5 percentage points. Error margins higher among subgroups.
A nationwide Washington Post-Kaiser Family Foundation poll asked more than 1,300 front-line health-care workers to describe the hardest part of working during the pandemic in their own words.
Topping the list were fears of infection for themselves, their family members or patients, mentioned by 21 percent of health-care workers.
[What seven ICU nurses want you to know about the battle against covid-19]
An additional 16 percent said wearing PPE was the hardest part of working during the pandemic. Some cited discomfort and overheating from wearing masks and other protective equipment throughout their workday, while others said masks detracted from the personal connections they seek when working with patients.
New and changing rules and safety protocols were also high on the list of challenges, with 8 percent saying these were the hardest part of going to work during the pandemic. Many cited frustration with rules themselves, as well as challenges getting patients and others to follow them.
An additional 7 percent said being overworked was the hardest part of working during the pandemic, with many feeling exhausted as they put in extra hours, covered for sick co-workers and coped with limited resources and dying patients. The poll found that among hospital workers, 56 percent said their workplace reached overcapacity for ICU beds or places to treat critically ill patients at some point during the pandemic.
[A Brooklyn ICU amid a pandemic: patients alone, comforted by nurses and doctors]
Five percent of health-workers said their hardest challenge was seeing patients who were isolated from visitors or family due to safety precautions. Most health-care workers said they provided direct treatment to covid-19 patients, and a quarter of all health-care workers had at least one patient die of the disease.
[A mass casualty event every day]
The Post-KFF poll found working during the pandemic was particularly stressful for younger health-care workers. Among those under age 30, 75 percent say worry or stress related to the coronavirus had a negative impact on their mental health, as did 71 percent of health workers in their 30s, a figure that fell to 40 percent among health-care workers ages 65 and older.
Nearly 7 in 10 health-care workers ages 18-29 and about 6 in 10 of those ages 30-39 feel burned out going to work, compared with less than half of those ages 50 and older.
[Inside a California hospital struggling to keep pace with the pandemic]
Even before the pandemic, experts had grown increasingly worried about the problem of burnout in health-care workers, including symptoms such as emotional exhaustion, cynicism, loss of enthusiasm and joy in their work, and increasing detachment from their patients and their ailments. Studies have shown burnout among health workers often results in increased risks to patients, malpractice claims, worker absenteeism and turnover, as well as billions of dollars in losses to the medical industry each year.
Despite the enormous stress they have borne through the pandemic, the survey finds most health-care workers also feel positive emotions about going to work. A 76 percent majority say they feel “hopeful” going to work these days, while 67 percent feel “optimistic,” and 63 percent feel “motivated.” Even among health-care workers who say their mental health has been hurt by the pandemic, most say they also feel hopeful, optimistic and motivated.

Washington Post-Kaiser
Family Foundation poll
Most health-care workers feel hopeful and motivated going to work, but also burned out
Q: Would you say you feel _____ about going to work these days, or not?
Percent of health-care workers
saying “yes” for each
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3.5 percentage points.

Washington Post-Kaiser Family
Foundation poll
Most health-care workers feel hopeful and motivated going to work, but also burned out
Q: Would you say you feel _____ about going to work these days, or not?
Percent of health-care workers saying
“yes” for each
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3.5 percentage points.

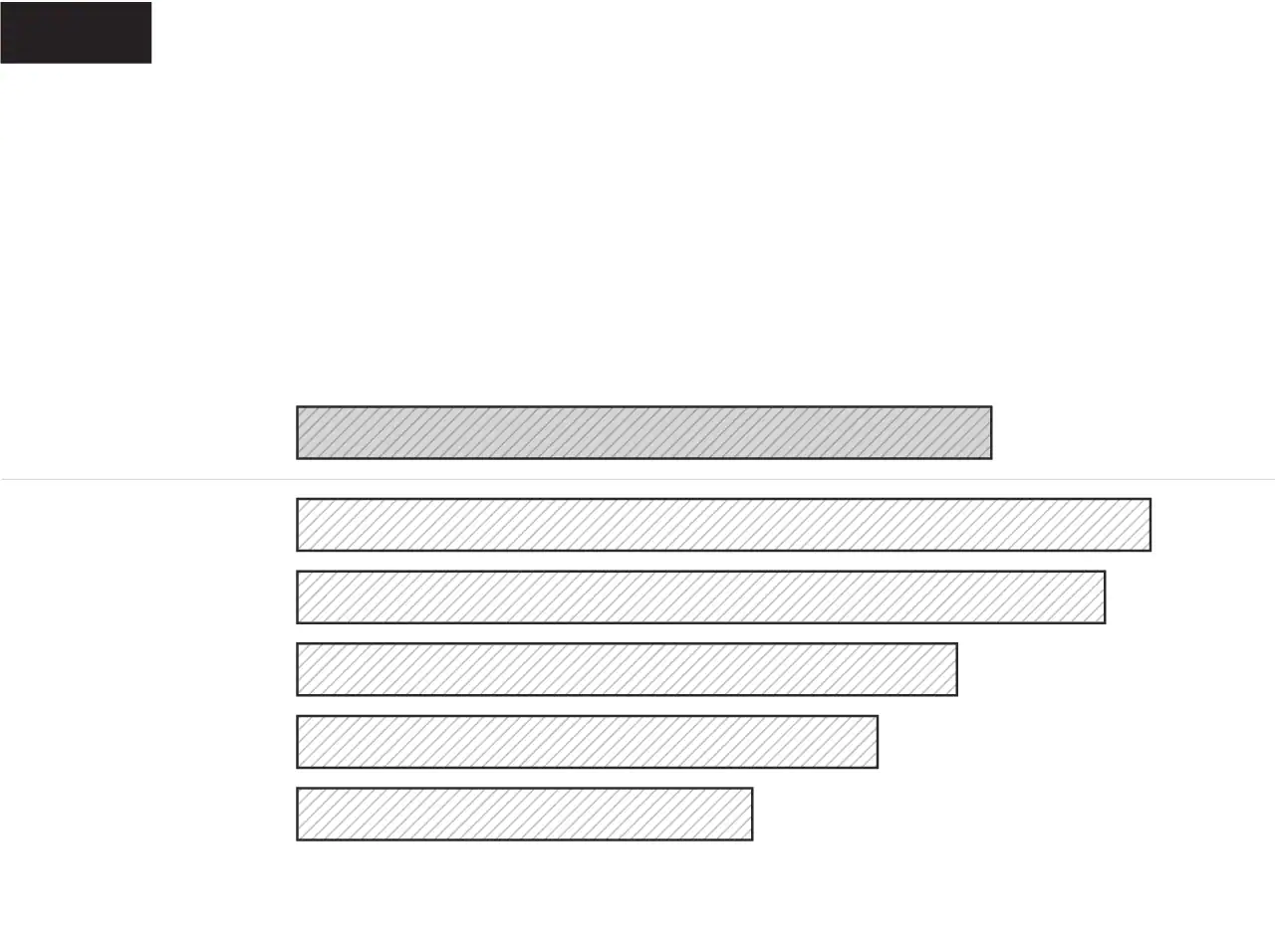
Washington Post-Kaiser Family Foundation poll
Most health-care workers feel hopeful and motivated going to work, but also burned out
Q: Would you say you feel _____ about going to work these days, or not?
Percent of health-care workers saying “yes” for each
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3.5 percentage points.

Washington Post-Kaiser Family Foundation poll
Most health-care workers feel hopeful and motivated going to work, but also burned out
Q: Would you say you feel _____ about going to work these days, or not?
Percent of health-care workers saying “yes” for each
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3.5 percentage points.
Emily Guskin, Lucio Villa, Naema Ahmed and William Wan contributed to this report.
About the poll
The Washington Post-Kaiser Family Foundation Survey Project is a partnership combining survey research and reporting to better inform the public. The Frontline Health Care Workers Survey is the 35th in the series. It was conducted in English and Spanish from Feb. 11 through March 7, 2021, among 2,298 adults 18 and older, including an oversample of 1,327 health-care workers living in the United States. Front-line health-care workers were defined as those who work in a health-care delivery setting in direct contact with patients or their bodily fluids, which roughly aligns with the type of health workers who were prioritized in the initial phase of coronavirus vaccinations. The survey was conducted online and by phone, with the majority of the overall sample drawn from the SSRS Opinion Panel and the Ipsos KnowledgePanel, which are probability-based panels recruited through random selection of U.S. households. A small percentage of interviews were conducted by recontacting respondents who identified as health-care workers in recent polls by SSRS and KFF. The combined landline, cellphone and Web samples were weighted to match demographic distributions of the U.S. population and the adult health-care-worker population. Demographic benchmarks for health-care workers were derived from an analysis of SSRS and KFF national surveys from December 2020 and January 2021. The general-population sample was weighted in accordance with the 2019 American Community Survey and the National Health Interview Survey. The results among the sample of the general population of U.S. adults has a margin of sampling error of plus or minus four percentage points, and the margin of sampling error is plus or minus three percentage points among the sample of health-care workers. Sampling, data collection, weighting and tabulation were managed by SSRS in collaboration with The Post and KFF researchers. The project team from KFF comprised Mollyann Brodie, Ashley Kirzinger, Audrey Kearney and Liz Hamel. The research team from The Post comprised Scott Clement and Emily Guskin.










