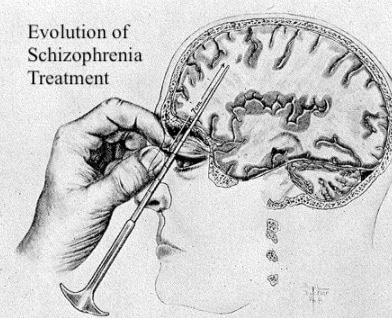
Schizophrenia has been around since the dawn of time but actually treating it has only been around the past 100 years. In this episode host and schizophrenic Rachel Star Withers takes you through the dark and disturbing evolution of schizophrenia treatments. From systematic euthanasia to hydrotherapy, electroconvulsive therapy to the infamous lobotomy.
Were these doctors “mad scientists” torturing the mentally ill or were they the only ones trying to help a population of people seen as a burden?
About our Guest
Miriam Posner is an assistant professor at the UCLA School of Information. She holds a Ph.D. in Film Studies and American Studies from Yale University. She is a digital humanist with interests in labor, race, feminism, and the history and philosophy of data. As a digital humanist, she is particularly interested in the visualization of large bodies of data from cultural heritage institutions, and the application of digital methods to the analysis of images and video. A film, media, and American studies scholar by training, she frequently writes on the application of digital methods to the humanities. She is at work on two projects: the first on what “data” might mean for humanistic research; and the second on how multinational corporations are making use of data in their supply chains.
Articles:
The Case of the Missing Faces
http://miriamposner.com/blog/the-case-of-the-missing-faces/
Frequently Asked Questions About the Lobotomy
http://miriamposner.com/blog/frequently-asked-questions-about-lobotomy/
Highlights from “Evolution of Schizophrenia Treatment”
[04:00] “Schizophrenia” as a term is first used
[05:00] Views of the top mind of the time
[07:00] Euthanasia of mental patients
[08:22] Nazi Germany’s plan to eradicate schizophrenia
[13:40] Mad Scientist or Helpful Doctor?
[14:00] Fever Therapy, Sleep Therapy, Insulin Coma Therapy, Hydro Therapy
[19:00] Seizure Therapies, Electroconvulsive Therapy
[23:00] The Lobotomy
[31:30] The First Antipsychotic
[36:00] Interview with Miriam Posner Ph.D.
[50:00] Walter Freeman’s Views on the Lobotomy
[1:03:00] Rachel’s Thoughts – it’s not the story of the patients
Computer Generated Transcript of “Evolution of Schizophrenia Treatment”
Editor’s Note: Please be mindful that this transcript has been computer generated and therefore may contain inaccuracies and grammar errors. Thank you.
Announcer: Welcome to Inside Schizophrenia, a look in to better understanding and living well with schizophrenia. Hosted by renowned advocate and influencer Rachel Star Withers and featuring Gabe Howard.
Sponsor: Listeners, could a change in your schizophrenia treatment plan make a difference? There are options out there you might not know about. Visit OnceMonthlyDifference.com to find out more about once monthly injections for adults with schizophrenia.
Rachel Star Withers: Welcome to Inside Schizophrenia. I’m your host, Rachel Star Withers here with my wonderful co-host, Gabe Howard. How are you doing today, Gabe?
Gabe Howard: I am doing great. As always, thanks for having me.
Rachel Star Withers: I am excited about today’s episode; I feel like we’re going to talk about some really interesting stuff. I was about to say cool. But maybe, maybe interesting would be a better descriptor.
Gabe Howard: I don’t think that you can have a fully fledged conversation about mental illness without the history, and part of that history is the evolution of treatments. And these treatments were often used for the sickest of the sick psychosis, schizophrenia. And we’re going to talk a lot about lobotomies because it’s, I think everybody’s heard of it, but I don’t think people really understand it.
Rachel Star Withers: Correct. I mean, myself, look, we’ve been doing this podcast for two years, and before that I’ve made numerous videos and other types of media about schizophrenia. And yet I learned so much when I was doing the research for this episode, things that I was like, oh, what? I’m just surprised I’ve never heard that before. What blows my mind is everything that we’re talking about is in the past, you know, 100 years. This isn’t like, well, back in the 1500s, they thought, well,
Gabe Howard: Right.
Rachel Star Withers: It’s back in the 50s, you know,
Gabe Howard: Yeah, yeah,
Rachel Star Withers: Like people are still alive.
Gabe Howard: Our grandparents are still alive,
Rachel Star Withers: Right? Yeah. Like, it really isn’t that long ago. And that’s blown my mind learning about the evolution of the treatments to where we’re at now.
Gabe Howard: It’s blown my mind, too, because when we think of something like a lobotomy, we think of One Flew Over the Cuckoo’s Nest, and as anybody who’s listened to us long enough has heard us say, don’t get your understanding of schizophrenia from pop culture. Yet we fell right into the trap. We were like, well, we understand lobotomies. Why we saw it on TV. Even at our level, Rachel, we’re still realizing that there’s just so much to learn. It’s a lot more complicated than we thought.
Rachel Star Withers: Yes, even finding a guest for today’s show that turned into being quite the hunt.
Gabe Howard: So hard.
Rachel Star Withers: I didn’t think so. You know, the title and how I reached out to different professors and doctors was we’re talking about the evolution of schizophrenia treatments. And I’m looking at people who literally teach classes on the evolution of psychiatry over the past 100 years. I’m like, I feel it fits right in there. And so many didn’t feel comfortable talking about these treatments. And our wonderful guest who we’re going to hear from later, I’d say she’s not who you would expect. She’s a digital humanist, which I didn’t know what that was. But she’s actually like one of the best people to talk to about lobotomies. And she blew my mind. She was totally awesome. So she’s coming up a little bit later.
Gabe Howard: I feel like we should point out that Miriam Posner is also an assistant professor at the UCLA School of Information. She studied this like she’s got a degree in this. It was fascinating, both everything that she said and the number of people that just didn’t want to talk about this on record for some reason. Like you said, it’s don’t you study this? Yes. Do you teach classes on it? Yes. Do you have a Ph.D. in this? Yes. Do you want to talk about it? No. Why not? It shows you that the misinformation is allowed to continue because so many people are like, well, it’s kind of something that we don’t want people to understand. It was confusing. So we were very excited for Ms. Posner to come on.
Rachel Star Withers: Well, before we can get into all of the kind of crazy treatments that came out and have been shown in the media, we need to talk about how schizophrenia was seen. The first time schizophrenia comes up is 1910. A Swiss psychiatrist coined the term schizophrenia, which in Greek meant split mind. What he meant was like a loosening of the thoughts, your thoughts splitting away. But of course, that very quickly became misinterpreted as a split personality and that has stuck with schizophrenia since 1910, that confusion. Which is just crazy to me, it’s like, man like even in the beginning they knew that was a bad name, but we’ll stick with it. The following year, one of the top psychiatrists described schizophrenia as the senility of youth. And basically you were going to be retroverting with your brain deteriorating. During the same time, we have Sigmund Freud, who also quite famous. He revolutionized for better and worse psychology. And a lot of his theories and stuff are still very prominent today. And Freud had a lot of opinions about people’s schizophrenia. That they could not handle reality and their paranoid delusions are motivated by unconscious homosexual impulses.
Gabe Howard: Paranoid delusions are motivated by unconscious homosexual impulses? That Rachel.
Rachel Star Withers: I know he just he kind of hit multiple offenses, so, like, I’m just going to offend everybody in one sentence. He also described people with schizophrenia as they would eventually revert back to an infantile state of around six months to six years old. So you have to understand, as we are rolling into the beginning of the 1900ss, the top minds at this time are not hopeful. They saw schizophrenia as something that those people, they’re like adult babies. Their minds will just get worse. There is no oh, we can treat this. Oh, let’s find a way to help. It’s nah, no, these people are terrible. That’s a lot.
Gabe Howard: It is a lot, and they categorize them in a way as to make them others. They’re other, it’s OK to do whatever we want with them because they are the worst society has to offer. They stopped short of calling them evil because they said they’re the worst society has to offer because they’re sick. But let it be known everything was up for grabs because I think society didn’t really care about them very much.
Rachel Star Withers: Society painted people with schizophrenia and other serious mental disorders at that time as a huge burden, you know, most families were ill equipped to help their family members, so mental institutions were their only options. And then at the mental institutions, you have doctors who are following, obviously, what the leaders of the country are telling you. And many of them did see euthanasia as a mercy killing. Some thought that, well, like these different psychiatrists have said, these people can only get worse. So we should probably kill them now so that they can avoid suffering. And a lot of mental institutions had a death rate of 30-40% a year. That’s a big death rate. You know, if you’re going to a hospital, you might rethink that hospital.
Gabe Howard: Well, yeah.
Rachel Star Withers: And this isn’t advertised, like they’re not openly saying, hey, you could be one of them, but that’s like low key what was happening.
Gabe Howard: And there’s reports out there like a mental institution in Lincoln, Illinois fed its incoming patients milk infected with tuberculosis. They were just experimenting on people with schizophrenia. And once again, want to point out, this is 1950.
Rachel Star Withers: And at the same time, we also have sterilization was huge in the U.S. Many states had forced sterilization of any patients in mental institutions. Throughout today’s episode, Gabe, I keep getting thrown off by the fact that so much of this stuff was on women. I would think sterilization. I honestly, I think men. But the majority was they sterilized the women because they’re like, we have to stop the babies. If you think about it, though, guys can make a lot more babies like than a woman.
Gabe Howard: Yeah.
Rachel Star Withers: But yes, so a lot of times when women came into mental institutions, that was the first thing that happened. It was not the cleanest, nicest ways of doing things. It was done as cheap and quickly as possible. Unfortunately, this is all over America. And at the same time, Germany is beginning in the Nazi era. I have done a lot of research into the Holocaust. I’ve actually been through the Auschwitz camps. So the fact that I didn’t know this stuff coming up is bizarre. But Germany, Adolf Hitler specifically, they really liked our eugenics programs and they decided that schizophrenia was a hereditary trait. And Germany embarked on a plan to eradicate schizophrenia, which sounds great. You know, that’s like, hey, you guys, we’re going to do this. They formed an organization called the Charitable Foundation for Curative and Institutional Care. That sounds wonderful.
Gabe Howard: Right, on the surface, it sounds OK, we’re going to eradicate schizophrenia, the name of the organization is good. And remember at the time when this was going on, we didn’t understand that Nazis were bad yet.
Rachel Star Withers: And this program, depending on the different years, it was 70-100% effective at eliminating schizophrenia in the German population. So the way this would happen was if you are thought to have schizophrenia, you would have to be assessed by three different doctors. If two of them decided you had schizophrenia, then you were sent to be euthanized. And a lot of these people were children. They wanted to catch it as young as possible. So they’re trying to find, you know, schizophrenia in children, which is very hard nowadays, you know, and you have two doctors and knowingly like, yep, this one’s out. To handle this is that they started building extermination centers in the main six psychiatric hospitals and those would later become the concentration camps. That blew my mind. I didn’t realize that basically, concentration camps started at psychiatric hospitals. I’ve just never been told that before. They also did different programs to see how little you could feed the schizophrenics, slowly starving them to death, how much they could work. And they took all this data that they learned and then used it not many years later on the people in the concentration camps. It’s easy to be like, well, Rachel, of course, those are Nazis. They do crazy things. And it’s easy to just sweep this all under the rug as like Nazi bad stuff.
Rachel Star Withers: But it wasn’t just them. In 1934, the Journal of American Medical Association, they actually did a report on the German eugenics and pretty much went on and on about the expected benefits. One of America’s top psychiatrists praised Hitler’s program and also one of the most renowned neurologists in America at that time warned that American mothers might respond with guilt over killing their mentally ill children. And he suggested that there be public education to help them overcome the emotional resistance to euthanizing their children. That’s the top neurologist. He was also the president of the American Neurological Association. He was on the board of the American Psychiatry. Like, this is the top and they’re talking about killing children very openly. And these are the main journals that are going to all the doctors. So everybody, everybody thinks at this time, you know, the only way to deal with this is through extermination, euthanasia. I didn’t realize how intense, I’m going to say, the belief was. I kind of thought, you know, yes, a few back alleys, you got some mad doctors kind of playing around wanting to kill off people. But no, these are the leaders of the medical community at that time.
Gabe Howard: So here’s what we have, we have people utilizing science and data and listening to experts in the field saying that this is the best course of action and the correct response is to say no, the doctors, the researchers, the data, the science, it’s all wrong. This is not the way that we should be treating human life. We find ourselves in a situation here now in 2020 where we’re trying to get people to listen to data, science and doctors. But again, it was less than 100 years ago that stuff like this was going on. And you can see where this creates a ripple effect in the trust of the medical establishment. You can see where people who are diagnosed with these illnesses, when they think back to how they were treated in the 50s, the 30s, again, this is all in America less than a hundred years ago. And you, you ask why people don’t want to trust or rely on their diagnosis? Well, there’s better than average odds if you’re Rachel and I’s age, that our grandparents know somebody who was honest about their illness and was institutionalized for life, or worse. It’s made it very difficult to move forward. And as we’re listening to this and as Rachel continues explaining the evolution of the treatment of schizophrenia, maybe being worried about a schizophrenia diagnosis for fear of stigma and discrimination is not just about being called names or not getting a job. It’s not too far in our history that it was literally a matter of life and death.
Rachel Star Withers: And I think what society has grabbed on to is all of the crazy treatments, they make great horror movies that kind of criminalize all of it. But what I learned is that the doctors who are doing these treatments, many ill advised, they’re the only ones actually trying to help. Yes, some of it is kind of crazy. And why would you think that would help? They’re the only ones, because the major medical minds are saying don’t even treat them. It’s pointless. So me coming to, I guess, that realization, Gabe, that was kind of hard on me because you see these different people and you think, well, they were just torturing people with schizophrenia, doing these terrible things, but at the same time, they were the only ones doing any therapy, trying anything. They were the only ones giving these people relatively a chance. Some of the crazy ones, and this one just blows my mind, fever therapy. So they would actually like inject you with sulphur or different oils to make you have this horrible fever. Now, the reason they did that is that they noticed that people who have malaria don’t have psychotic symptoms. I mean, I feel that’s a stretch. But OK, something about a fever makes you less psychotic. Another one they did was deep sleep therapy. And that’s where they would, like, put you to sleep for days, sometimes weeks. Very close to that is insulin coma therapy. They would just repeatedly inject psychiatric patients with large doses of insulin and they would put you into a coma and the coma would only last for like an hour. But you would do about 50 to 60 of these comas in six weeks, up to two years, just repeatedly going in and out of a coma like that. That’s amazing to me. What kind of life is that?
Gabe Howard: I don’t think it’s much of a life at all, right? I think this is an excellent example of where the phrase the treatment is worse than the illness comes from. It sounds terrifying. It sounds traumatizing. It sounds painful. And it wasn’t particularly effective. Correct?
Rachel Star Withers: And as we’re going to see as we talk about some of these treatments, parts of it did. That’s where the issue is. Parts did work. Trying to separate those parts, you know, unfortunately, led to a lot of I would describe torture to a lot of people trying to get to those. And many of them were psychotic at the time and had no clue what was happening to them or could consent to it in any way or it was a family situation. You look at so many children actually were put through all of these treatments. You know, when we think back to horror movies and stuff, it’s always adults. When you have a child that you’re doing this to, you know, it stops being a horror movie. This just becomes something really just bad and gross. Why would you even do that? And to realize that was the truth in it is that it happened to the majority. Any children that were thought to have schizophrenia. Another one is hydrotherapy. So, Gabe, if anyone’s seen the new Netflix show, Ratched, they actually do hydrotherapy and I’ve never seen it before. I was like, what is this? But really interesting. And that’s where they would either put you in really, really hot water or really, really cold water. Sometimes you would literally be like strapped into a bathtub. You could be left in that bathtub for days. You know, when you think about a continuous bath at first that sounds nice. But when you’re like you’ve been in hot water for three days, I mean.
Gabe Howard: It’s terrifying. Each one is more terrifying than the next, and you’re not done.
Rachel Star Withers: Oh, no, I would say these are the softball ones. Oh, you have to understand, but there was logic to it. They found that warm water helped with insomnia. It helped with people who were suicidal and it helped calm people down. Cold water, freezing water was usually used on people who were psychotic. There was something about the cold water, slowed the blood flow down to the brain and decreased mental activity. You know, you see different bits of what was working, unfortunately, horrible ways to get to those little bits. One of the things with the hydrotherapy is that one of the mental institutions actually would chain the psychiatric patients to the wall and they used a fire hose on them.
Gabe Howard: Just wow.
Rachel Star Withers: It’s so easy for any of these treatments to turn into torture so quickly.
Gabe Howard: Rachel, I have to ask, though, you realize that if you would have been born 100 years ago, this is the treatment that would have been given to you. Rachel, as somebody who lives with schizophrenia, how are you feeling right now?
Rachel Star Withers: It makes me think back to around, I guess, sixth grade, you know, middle school age. But that was the first time around then that my parents took me to see a counselor for outbursts and issues. You know, I sat there. I didn’t like the woman. I don’t remember anything about it. I remember not liking her. We saw a couple of different ones, some religious, some normal. And I think had that been the situation, let’s say in the 40s, I could have been. All right, let’s just spray this, what, 12 year old down with the fire hose, that that would have been probably what could have happened.
Gabe Howard: Yeah, they would have sprayed you down with the firehose. How do you feel about the idea that your parents might have chosen to spray you down with a fire hose and then have been told by the top psychiatric doctor in America that they just needed to manage their emotions while watching you get sprayed down with the firehose? Actually, he said, manage your emotions for you to be euthanized, but let’s move it back a layer and just say manage your emotions to watching their 12 year old be sprayed down with a firehose.
Rachel Star Withers: It’s mind blowing.
Gabe Howard: It’s terrifying.
Rachel Star Withers: So the issue now is that we’re starting to find more of what works, but still how do we get to it is the issue. And that’s where seizure therapies came in. And the way they realized this was actually a Hungarian pathologist, he noticed that people with epilepsy almost never had schizophrenia and that after an epileptic seizure, those people tend to be very happy. So the idea was, well, if I give people with schizophrenia seizures, that should help them. There is numerous ways they went about this. It started with doing lots and lots of pretty much injections with drugs. They found they could go back to the insulin and inject you with tons of insulin. It would give you seizures. These are all horrible things and obviously lots of side effects from being injected with just tons of random chemicals. What happened was they found a much better way. I like the story of how this came to be because there’s just so much of this stuff is red flags, electroconvulsive therapy, where electricity is shot through the brain to induce a seizure. The first human trial was in 1938. So a while ago. But the idea was the doctor had learned that pigs before you like kill pigs to eat them, like at a big plant, you give them an electric shock and they pass out. And somehow that was like, you know what, I think that can help the schizophrenics. And I don’t know, just like you were at a pig plant, that, that’s where they
Gabe Howard: Wow,
Rachel Star Withers: What?
Gabe Howard: Wow.
Rachel Star Withers: So that’s where electroconvulsive therapy originated. Fortunately, in the 40s, they did it quite often. And at that time, they didn’t use any muscle relaxers or anesthesia. So a lot of people were fully aware as they’re being shocked, they broke bones. They had people holding them down. And it was a very intense procedure to go through. By the 50s, they had now learned to do a modified version where they would put you to sleep and give you muscle relaxers. So for about ten years is the real bad horror stories. And then in the 50s is where, OK, we’re going to keep doing this, but we got to find a better way. And I think really that was a good changing point in mental health of we need to find better ways to do this.
Gabe Howard: I guess it’s important to understand, ECT, electroconvulsive therapy is actually still a treatment that’s used today. It works very well. In fact, you’ve had ECT, so you’ve named off a lot of very scary things and things that they no longer do. But all of that scary list, one of them has stuck around.
Rachel Star Withers: Yes, it’s always a very touchy subject because I have people reach out to me who only see it as torture because of what happened to so many people. And I do agree it was used horribly. Another thing they like to do with children is shock them twice a day for 20 consecutive days. I was an adult when I had ECT and I can’t imagine someone doing it to a child. I had it for two weeks, three a week. There was so much bad stuff with ECT. But where it was in the 40s to where it is now is different. If you ever talk to my mom, she will always tell you how that was like a major change for me. For me it helped and I’ve looked into getting it again. So I understand it’s a very, you know, controversial thing. Does it work on some people? Yes. That segue leads us into, Gabe, one of the most notorious treatments, the lobotomy. What’s crazy is that when you hear lobotomy, you think of schizophrenia. But when they were actually doing them, you got a lobotomy for like everything. It was for ADHD. It was for manic episodes.
Rachel Star Withers: It was for depressive episodes. It was for people who didn’t fit in. The lobotomy was the go to. But looking back in history, you think, oh, man, that’s for that’s what they do to schizophrenics to get them under control. That’s been the enduring image. So lobotomy, it’s actually called psychosurgery. And that is any time that surgery is done on the brain in order to relieve a mental disorder. And a lobotomy is one of the psychosurgeries. Psychosurgery is still performed today. Versions of the lobotomy still take place today. Is any of it like it was in the 30s on to 60s? No, it is the completely different. The first form of a lobotomy was actually done they would drill holes in the skull and they would then inject ethanol into it. And the goal was to destroy some of the white matter in the frontal lobes. And for whatever reason, they learned that destroying white matter in the frontal lobes somehow makes people calmer. They notice that when, after the wars, the soldiers coming back who had had brain damage to the front of their heads, their personality had changed. So that’s where the whole thought process came of why we should, you know, start sticking holes in people’s brains.
Gabe Howard: I understand what you’re saying, but the exact words were used is that doing that psychosurgery made people calmer. You didn’t say made people better or allowed people to use their best lives. It very much seems like this was a mechanism of behavioral control, not necessarily what was best for the patient.
Rachel Star Withers: And that that’s where we get into so much interesting things, which Miriam Posner will help us understand some of that because, yeah, it’s a double edged sword. There are so many people who swear by it and it helped them. It’s the reason they were able to go have lives. And then you have other people who, for one, died. Quite a few people died from it, not just because they had pieces of their brain stabbed, but because of the conditions. Many got meningitis. Walter Freeman, one of the main neurologists who like to do the lobotomy, he didn’t use gloves or a mask and they were already using those back then.
Gabe Howard: Wow.
Rachel Star Withers: So you have people that are dying. And Walter Freeman, one of the things he’s known for is the ice pick lobotomy. And he figured out a way to avoid drilling holes in the brain. So at first, it sounds great. We don’t have to drill pieces in the skull. I found a way around that, that’s much quicker, much simpler. It involves an ice pick.
Gabe Howard: I, that’s, that’s not better.
Rachel Star Withers: No, it’s not, you know, the mental process of all of these always starts out good and then suddenly takes a wrong turn. And yes, he discovered that you could use an ice pick to go through the eye cavity. It is intense to watch. There’s lots of YouTube videos you can find of these surgeries. I would say after watching so many videos, it occurred to me that no movie has ever come close. There’s something about watching these black and white videos of them taking an ice pick to the person that is so unnerving. It’s not like any kind of crazy images from movies where they do it. It’s much more real and intense. And the majority of lobotomies were done on women and children. So you had a kid with ADHD or suspected with schizophrenia or didn’t fit in and was weird? Lobotomy. That was the go to
Gabe Howard: Wow.
Rachel Star Withers: It’s a very dark time in psychiatry in general. Did it help some people? Yes. Going into it, did it calm people down? So, Gabe, this actually it makes me think back because, yes, most of these treatments were to come and help people get control of their schizophrenic. That’s kind of what it was like. This is to help you get control of your loved one. It definitely wasn’t to make the loved one better. But I look back at my ECT. And what did it do for me? It took away my depression. It took away a lot of my OCD. My hallucinations were much harder to deal with. I would say I was not controllable. So did ECT do that to me? I think it did. It helped me, yes. But did it essentially make me calmer? Yes. So, I mean, this is a moral dilemma for me as I’m learning more and more about this, because I’m like I see both sides of it and I don’t even know where I stand when I think about that.
Gabe Howard: I certainly understand the idea of something can be two things, I mean, if you are calmer, if you are easier to talk to, if you are able to follow the rules, that’s definitely a benefit to friends, family, if you’re in the hospital, staff or society at large. But there’s also something to be said for that’s best for you as well. Right? Like, I guess that’s what I’m saying. It’s just you do go back and forth on whether ECT just made you better, made you better for your friends and family. But you’re making these choices on your own.
Rachel Star Withers: Right.
Gabe Howard: You like to have your home life be serene and calm and stable. Right. So just because your family benefits from your decisions doesn’t retroactively make them not your decisions. But in the case of some of these treatments, you don’t even know where you are. What was the one where they make you sleep for two years? They wake you up every four weeks to like what, rotate you? What kind of a treatment is that? It didn’t make you better. When you hear stuff like this, you can see why people are terrified of the treatments for schizophrenia, because, again, it wasn’t that far in the past before the outcome of treatment was just you obeyed and made life easier for the people around you, but your quality of life was nonexistent.
Rachel Star Withers: And especially there’s so much around the lobotomy, it was thought to be around 50% effective, which again, for the time period, your other option is death or pretty much just going on as you are and probably becoming homeless or other things and eventually dying of those reasons. So if someone offers you a 50% chance of being normal, that’s I mean, I’m like, well, that’s a pretty good deal. That’s a good deal. It had a death rate of around 14%, you know, so a lot of the people willingly had this done. They were desperate. They knew what could happen. It was very well known that your personality could change. You might have to relearn how to do everything. The neurologist, Walter Freeman, who did most of these, he called it a surgically induced childhood. They know what they’re doing. I don’t think they looked at anyone as this is going to make you better and take away this thing. It’s no, it’s going to make you more childlike. And you go from there. I don’t know. I worry because when I read his thoughts and a lot of the doctor’s thoughts, like, it’s like you kind of knew you weren’t doing a good thing. I just,
Gabe Howard: It’s what it sounds like, right?
Rachel Star Withers: Yeah. He described one of his patients who was a success story, he said following her lobotomy, she was a smiling, lazy, satisfactory patient with the personality of an oyster.
Gabe Howard: That’s not successful treatment.
Rachel Star Withers: It’s like, wait, what? You know, and later he had another patient he actually wrote notes about and said that the best that can be done for a family sometimes is to return the patient to them in an innocent state, much like a household pet.
Gabe Howard: Literally, it’s an incredible quote that the best that you can hope for your patient is to give them back to their family. He actually said as a veritable household pet. That’s the exact quote from his note. Like, that’s what the doctor thinks about the patient. Like, it is terrifying.
Rachel Star Withers: And that’s a success story,
Gabe Howard: Right.
Rachel Star Withers: That was a success story. That’s thing, it’s just like he’s like, this is good. He is promoting this.
Gabe Howard: Yeah, he’s proud of himself.
Rachel Star Withers: Yes.
Gabe Howard: Wow, wow. But luckily we moved past that, we get to medication therapy. The very first antipsychotic came out in the 1950s, and this is what I think people think of now when people think about the treatment for schizophrenia, now they think of antipsychotics. And those came onto the scene in the 1950s. Tell us about that, Rachel.
Rachel Star Withers: That was pretty much the revolution. Now, you don’t have to have that weighing on your conscience of having to stab your family member with an ice pick. It is they could take a medication and they can go they can get a bunch of pills and then come home and take them one a day, etc. So you also had people could come back and live with the family more. You didn’t have to worry that any of the procedures were going to leave them with brain damage, having to relearn how to read and write. Now, the way they came up with this for the first antipsychotic was it was used as a histamine. The point was that they noticed it had a calming effect. It all goes back to making people calmer. That was where antipsychotics started, was making people calmer and it went on from there. And at the same time, ironically, there is this crazy new form of psychotherapy that was gaining speed called cognitive behavioral therapy. And that was the first psychotherapy they had found that actually helped schizophrenics. They had tried different ones in the past. But there’s something about the cognitive behavioral, it really helped people with schizophrenia. So this was a big turning point.
Gabe Howard: And the medication is still the standard today, I mean, you know, medication therapy, peer support, but the big one, the one that everybody thinks of when managing schizophrenia is medication. And I think people are unaware of, you know, just how recent of a discovery that was. And it’s important to understand that the first one came out in the 1950s, that the first of anything, you know, the first cars were not so great.
Rachel Star Withers: Yes.
Gabe Howard: They took time to perfect cars from when they were invented. And I would argue that we still haven’t perfected medication treatments for schizophrenia. Would you agree with that? I mean, there’s side effects. There’s issues. There’s still a lot that we don’t understand. New medications are coming out all the time. Research is ongoing. And I only bring that up because I think so many people are like, well, just take your meds, Rachel, and you’ll be fine.
Rachel Star Withers: It’s kind of like looking back at all these old timey treatments, it’s like you’re trying to figure out what works and just do that without all the other horrible things. Ironically, that’s where we’re still at now. Luckily, the side effects are not death as many times as it was back then or sleep for two years. But that’s just yeah, that’s just the evolution of these treatments. To get to where we are now a lot of that stuff had to happen.
Gabe Howard: Obviously, we want to make sure that our listeners understand that there’s just a lot going on, it’s not as simple as good versus bad or right versus wrong or any of that. There’s just a lot going on and it’s difficult to understand. But I think that sometimes when people think about this, they’re really quick to say, oh, why are you so worried, patient with schizophrenia? The doctors had their best intentions in mind. So we give the benefit of the doubt to the doctors for the mistakes that the medical community has made. Well, why don’t we give the benefit of the doubt to the patients who are leery of the medical community, given the number of mistakes that they’ve made? And I think that’s one of the things that is missing. When we talk about people with schizophrenia who are afraid of medical treatment, there’s an actual factual basis to be concerned about what they’re being told. This isn’t made up of whole cloth.
Rachel Star Withers: And now a word from our sponsor.
Sponsor: It can sometimes feel like another schizophrenia episode is just around the corner. In fact, a study found that patients had an average of nine episodes in less than six years. However, there is a treatment plan option that can help delay another episode: a once monthly injection for adults with schizophrenia. If delaying another episode sounds like it could make a difference for you or your loved one, learn more about treating schizophrenia with once monthly injections at OnceMonthlyDifference.com. That’s OnceMonthlyDifference.com.
Gabe Howard: And we’re back discussing the evolution of schizophrenia treatments on Inside Schizophrenia.
Rachel Star Withers: Yes, I absolutely agree, and that’s why we reached out to our guests today, Miriam Posner, to help us understand this side of psychiatry.
Gabe Howard: Without further ado, here is that interview.
Rachel Star Withers: We’re here speaking with Dr. Miriam Posner, and she’s an assistant professor at UCLA School of Information and she’s a digital humanist. Miriam, tell us what is a digital humanist?
Miriam Posner: It’s a field of study where scholars use and experiment with digital tools to explore humanity’s questions, and so it can look like a lot of different things for different people. But if you think about like maps to show the spread of a historical event or a network diagram to show how people were corresponding during, say, the Renaissance or even there are some experts in computer assisted text analysis who try to find patterns in text. So, yeah, so I’ve been part of that community for about a decade now.
Rachel Star Withers: So the reason we asked you to be on our show today is that you have spent a considerable amount of time studying lobotomies and you wrote some different articles. The Case of the Missing Faces, frequently asked questions about the lobotomy. Tell us a little about that part of your research.
Miriam Posner: What got me interested in lobotomy was that I’ve always been interested in medical images and the kind of work that medical images do to persuade people or affect our understanding of disease and patients. And a professor in grad school just happened to show the class a clip from a film that was made of lobotomy patients after they had had surgery. And the footage was just so affecting to me. It was one thing to read about the effects of lobotomy and what it was like to have a lobotomy. And it was another thing to watch the patients struggle to find themselves afterward. Those images really stuck in my head and I started wondering how many other images are there of people who had lobotomies and what was the point of images in the history of lobotomy? I was looking at how physicians were using photographs and film to make arguments about lobotomy. But along the way, I learned a lot about that episode in our history and also about Walter Freeman, who was the foremost exponent of lobotomy in the United States.
Rachel Star Withers: And can you explain to us the pictures that you had studied, the before and after photos? Tell us about those.
Miriam Posner: Yeah, one thing that really took me by surprise is that Walter Freeman was obsessed with taking before and after photos of his patients, he would routinely take a before picture of a patient before performing a lobotomy. And then even years later, he would come back and follow up with a patient to take an after picture. He was very dedicated to seeking out patients and he would drive across country to stop at people’s houses and take after photos of his patients. And I just thought, what? Like why? Like, why would you do that? And it was really surprising to me. And I thought, what did he think he was showing with these images?
Rachel Star Withers: What is your interpretation since you’ve been studying them? What is yours of looking at all these different photos?
Miriam Posner: Well, to Walter Freeman, I think that those before and after photos constitute proof that lobotomy was effective in treating patients’ mental illnesses. The kind of strange thing is, that to us, it’s not always clear what about the after picture is proof because it’s really hard to tell what exactly he was seeing that meant that the person was visibly cured. In order to understand why he thought those after pictures were effective, I had to do research about what constituted mental health to Walter Freeman and to other psychiatrists in the period where he was active. The signs of improved mental health are often things like putting on makeup for women, wearing appropriately feminine clothes, being surrounded by family, for men wearing a suit and working what Freeman thought was an appropriate job and even putting on weight was for him like an example of mental health.
Rachel Star Withers: Interesting, but those also seem like that’s something that could be easily staged for as far as the clothing, the makeup.
Miriam Posner: For sure, for sure.
Rachel Star Withers: I’m not an emotional person, but I was looking at the before and after photos of this woman, and it made me cry because the before photo was very almost like a mug shot. She looked
Miriam Posner: Yeah.
Rachel Star Withers: Kind of annoyed that this was happening. And the second one, she was smiling and it wasn’t like a big smile or anything, but her eyes to me, what grabbed me was her eyes. And it just made me cry because just what I went through with depression. Now, I don’t know the story behind it. That could have been one of the ones, Oh, and she’s happy but had to relearn how to walk. But just the photo itself to me was incredibly powerful, if you would have just shown me that. And it was like this is proof that it works. I’d be like, wow.
Miriam Posner: That’s something that hits me, too, is that these photos are actually emotionally pretty powerful to look at, but really probably not for the reasons that Walter Freeman thought that they would be powerful. He thought you could take a look at them and just be like, wow, that person got better. But just as you say, you feel like you can look in someone’s eyes and see that things are not OK, even though that’s not what Walter Freeman saw. But it kind of makes sense that the makeup and the dresses and markers of like appropriate gender presentation, that he thought that those were evidence of mental health just because of the way that psychiatrists like Freeman thought about mental health in the 30s and 40s. Mental health was not so much about a person’s insight or ability to articulate and identify their own feelings. It was much more about integrating the person into society in a quote unquote, useful way. Could the person hold a job? Could the person have a family and perform like a gender appropriate role in the family? Could the person show up to an event and not be disruptive? So that was mental health to him. It really wasn’t so much about a person’s feeling fulfilled as a human being.
Rachel Star Withers: I was very shocked to recently learn that majority of lobotomies were performed on women and even children. In your opinion, looking at the photos and now telling us this, that so much of it was the person playing the gender role correctly, why do you think more women had lobotomies? Was it that gender bias or is it just because women tend to seek help quicker than men do?
Miriam Posner: I don’t have an authoritative answer for you, but I can speculate a little bit about that. When the lobotomy first started being performed in the late 30s in the United States, it was reserved for patients for whom there was no or they believed there was no alternative. Patients with really intractable mental illness. But as the years went by, the indications for lobotomy expanded to include lots of other symptoms, things like depression, pain and inability to integrate into family and work. And it seems to me that it’s in that period of expanding diagnosis that women presented more often as candidates for lobotomy. And you’ll read case studies where it appears to a modern reader that the woman is unhappy with her lot in life. She’s not fulfilled by her role as a homemaker. She’s in an unhappy marriage. She perhaps doesn’t want to perform the activities appropriate to a woman during this period. And for some women, those signals became interpreted as depression that was severe enough to qualify her for a lobotomy. I don’t think that Walter Freeman or other lobotomists had an explicit policy of lobotomizing women more frequently. But I do think that they tended to interpret what they saw as maladjusted symptoms pretty loosely as making them good candidates for lobotomy.
Rachel Star Withers: As you spoke on, the lobotomy was used as a cure all for mental illnesses around that time, they didn’t have as much information on them. However, I think nowadays, when you look back on lobotomy, the disorder that’s most commonly associated with it is schizophrenia,
Miriam Posner: Mm hmm.
Rachel Star Withers: Why do you think that is? Why do you think that schizophrenia is, when they think of lobotomy, they think crazy person, screaming, schizophrenic? They don’t think depression. They don’t think ADHD. They don’t think, yeah, like you say, just not adjusting to the times, being oppressed.
Miriam Posner: Yeah, I do think that people sometimes have a mistaken understanding of the history of lobotomies, maybe because of the way it’s depicted in films. A lot of people assume that lobotomy was confined to the back halls of disreputable mental institutions, that it was disreputable physicians who performed lobotomies, that it was always a sketchy procedure. But what a lot of people don’t know is that during the heyday of lobotomy in the 30s and 40s, it was considered the top of the line, most modern and most effective treatment. Walter Freeman was on the cover of magazines. He was mentioned for a Nobel Prize. There was no sense that lobotomy was a weapon of cruelty. Lobotomy was understood to be the most current, up to date, scientifically precise treatment for mental illness. And I think people associate schizophrenia with being uncurable. So I think in people’s minds, because they believe schizophrenia is incurable, that lobotomy would be the most likely candidate for a disease. But while it was performed on people with schizophrenia, in fact, the indicators for lobotomy were actually a lot more broad than people suspect.
Rachel Star Withers: How has public perception changed as far as lobotomies and that type of treatment? Obviously 30s, 40s when Walter Freeman was at his height, yeah, that seemed like a go to. At what point did the public kind of start to pull away from this miracle cure?
Miriam Posner: One big rupture was the introduction of antipsychotic medication, chlorpromazine was introduced in 1954 and that really provoked a sea change in treatment of people with schizophrenia and related diseases. So suddenly there was another treatment that didn’t require biological surgical intervention and that could be fine tuned and didn’t seem quite as drastic as a surgical procedure. There was also increased interest in talk therapies around that time. Freeman’s brand of psychiatry, which was always most interested in biological organic causes for her mental illness, fell out of favor a little bit. And so as the years went by, it became more common for people to see lobotomy as a really brutal, inhumane treatment. But one thing that’s interesting about Walter Freeman is that he never really accepted that interpretation of lobotomy. He believed until the end of his life that lobotomy was the most appropriate treatment for people with intractable mental illness. And his interpretation of treatment with antipsychotic medication was that it was like a temporary solution to a problem that could be permanently solved by surgical intervention. Medication he thought was kind of a Band-Aid, but the real successful way to intervene would be to go in and separate the thalamus from the frontal lobe.
Rachel Star Withers: That’s interesting because we usually only see it from the side of the lototomy was a horrible, torturous thing, not the other
Miriam Posner: Mm-hmm
Rachel Star Withers: Way of him being like, yeah, the other option is like a Band-Aid. Very interesting. I think one of the most popular portrayals of a lobotomy was from the movie One Flew Over the Cuckoo’s Nest, and it’s known for its bad portrayals of mental hospitals, of people with mental illnesses, of showing electroconvulsive therapy in a very bad light. And, of course, in the movie, I’m sorry if you haven’t seen anyone listening. But, yes, a lobotomy takes place and he’s pretty much brain dead at the end. How do you think those massive media portrayals have affected research into psychosurgery and other types of mental surgeries?
Miriam Posner: I think that lobotomy often is interpreted as kind of a joke now, it feels like really distant in the past to a lot of people, and it is very closely associated with brutality and something that was performed in the like back wards of really brutal mental institutions. But it’s important if we really want to understand lobotomy to understand that a lot of people were on board with it. A lot of institutions and individuals thought that it was a good idea and there was a way in which it was part of a continuum of therapies that are called somatic therapies. So any kind of therapy that’s performed on the body. In many institutions, you’d start with a somatic therapy, like being tied to a bed and then continue on through this spectrum, through ECT or insulin shock therapy or being submerged in ice water. And when the patient failed to get better after this kind of chain of somatic therapies, they finally were seen as a good candidate for lobotomy. We tried everything and now it’s time for the real king of somatic procedures, which is lobotomy.
Rachel Star Withers: From all of your research, looking over Walter Freeman’s work and other aspects of lobotomy and portrayals with media, what is your overall take away?
Miriam Posner: What I like for people to understand about lobotomy is that the episode is not an aberration. It’s not the result of a couple kooky physicians who made miscalculations and somehow managed to sneakily lobotomize a lot of people. Instead, that’s science. That was mainstream science. That was considered the peak of good clinical practice at the time. And if we accept that’s true, then we have to accept that science can make some real drastic miscalculations and can inflict real damage on people just in the day to day course of doing business. So it’s not an aberration. It’s not a crime that people got away with. It was something that was endorsed at the highest level of the psychiatric profession.
Rachel Star Withers: Tell us what happened with Dr. Walter Freeman after the public and the medical community started to move away from lobotomies and it fell out of favor.
Miriam Posner: He never really accepted the rejection of lobotomy, and he was advocating for lobotomies until the end. He performed his last lobotomy in 1967 and shortly after that he was stripped of his operating privileges and was incredibly indignant about it. One episode that kind of sticks in my mind is that in order to make his case to the hospital board that he should be able to continue to perform lobotomies, in order to make this case, he brought a box full of Christmas cards from his former patients where they expressed thanks for what he’d done to them and concern for him as a human being. And so he emptied this box on the table and said, is this the result of a procedure that’s inhumane and brutal? Look at this. My patients are all grateful to me. And it’s in a way like for me, encapsulates just some of the weirdness of the whole episode and how confusing it is to try to understand what Walter Freeman thought he was doing. Because I really do think that he thought that he was fixing people and there were some people who did interpret what he had done to them or members of their family as a positive change. And he could never get his head around the idea that people didn’t see it that way anymore.
Rachel Star Withers: That’s a very powerful thought that, yeah, he saw it one way and all of the Christmas cards, the photos that he documented, and then, of course, I’m sure the actual people themselves. But then when you contrast it to the fact that his last lobotomy, the woman died and
Miriam Posner: Mm hmm.
Rachel Star Withers: So many people who became severely impaired, it’s very interesting when you think about
Miriam Posner: Yes.
Rachel Star Withers: The extremes of the lobotomies, how it worked out for everyone.
Miriam Posner: Yeah, nothing is ever black or white, and there are so many strange stories that still surprise me that pop up.
Rachel Star Withers: Given this kind of very dark area of schizophrenia treatment in the past, I know a lot of people could use this to not want to get psychiatric help today. Tell us your thoughts on that.
Miriam Posner: Well, I mean, they’re right that it’s a really sobering episode in the history of psychiatry and in thinking back about it and what it means to me today, one of the lessons that I hope that psychiatry has learned is that judging people’s mental health by their ability to integrate into mainstream society is actually really dangerous because there are a lot of reasons someone might not fit in. And to assume that they can’t fit in because something’s wrong with them is really damaging. And I think there has been a turn among psychiatrists to look at how patients themselves define health for themselves and to understand that mental health may not look the same for everybody and it may not look like psychiatrists want it to look for everybody. So the lesson is actually, I think, pretty simple, if difficult to actually realize. And that’s but you have to listen to patients, like you have to understand what their goals are, what their definition of health for themselves is. And you have to respect that for them, living a fulfilling life may look different than what we want them to think.
Rachel Star Withers: Is there any media that you suggest that you think really shows this treatment and is a good thing for laypeople like me to watch, to understand more?
Miriam Posner: There is a radio documentary called My Lobotomy, which is a long interview and a series of meditations by a guy named Howard Dully, who is still alive today and is one of the last people on whom lobotomy was performed. It was performed on him when he was a teenager. He talks about the experience of getting a lobotomy and how it still affects his life to this day. And it’s a really powerful documentary. And he also has a book that’s called My Lobotomy that is equally effective and moving. There’s a documentary, too, that’s called The Lobotomist that focuses more on Walter Freeman, the biggest cheerleader for lobotomy. What was going through his head? Why was he so convinced that lobotomy was the way to go? And talks a little bit about the context in which he was performing these procedures. Those are really good ways to get acquainted with how lobotomy was conceived of at the time.
Rachel Star Withers: Thank you so much for speaking with us today, Dr. Posner, about all this, so much good and bad when it comes to looking back over the different treatments for severe mental disorders just over the past hundred years alone. How can our listeners learn more about you and your work?
Miriam Posner: They can certainly check out my website, which is www.MiriamPosner.com, and I have a lot of materials about lobotomies there and a blog where I sort of talk about what’s preoccupying me now. And they can always get in touch with me on Twitter, too. My handle is @MiriamKP, and I’m always really interested to hear from people particularly who have experience with the mental health system and can help me understand what their experiences are like.
Rachel Star Withers: Awesome, thank you so much for speaking with us today, Dr. Posner.
Miriam Posner: My pleasure.
Gabe Howard: Rachel, she was awesome and I’m super glad that she agreed to be on our show. What was your biggest takeaway after speaking to Ms. Posner?
Rachel Star Withers: I enjoyed this interview so much. I enjoyed her so much, I think because she wasn’t the doctor, she wasn’t one of the typical psychiatrists that I had originally reached out to. She definitely came at this with a different viewpoint. And that was kind of interesting to see, you know, someone who wasn’t directly in the psychiatric community as a patient or as a doctor, counselor or whatever, to be able to say, look, this is my views of what happened over this time. It was very refreshing and it was different the way she spoke about things than I would say any other guests we could have picked.
Gabe Howard: I would agree with that. Her understanding of history was very commanding. You think you understand because everybody’s talking about it. But as a researcher, she just had this other level that I thought was very, very interesting.
Rachel Star Withers: Yes. Should we look into becoming digital humanists or is it too late?
Gabe Howard: I did not know that that was a thing, but she explained it well and it’s understandable. I think this is another example of how modalities and research and life moves forward. I mean, digital humanist wasn’t a thing 50 years ago, but it is now and it’s understandable how we got here. And I think that’s very analogous to where we are with the treatment of schizophrenia. There is trauma in our past. There’s a lot of trauma. And I do think that we need to do more to address that trauma. The general attitude is, well, we were doing that for your own good. Well, we were trying to help. And I do think that we need to openly discuss mistakes that were made so that we can have more buy in that these mistakes won’t happen again. I do think that she did an excellent job of making sure that people understood the history of this particular schizophrenia treatment and where we’ve come from. And I think that’s overwhelmingly positive.
Rachel Star Withers: When I asked her final thoughts about advice for seeking treatment for schizophrenia. I kind of meant it as like, you know, a closing type kind of squishy question. And when she responded, it kind of threw me off because she spoke to psychiatrists in her response and about the definition of health. I was just like, oh, OK. I thought she would be like, oh, the medical community has come so far, blah, blah, blah. But no. And that was kind of it made me think because I’m like, well, that was weird that she spoke to them. You know, I clearly would have spoke to other people with schizophrenia, I think most doctors and whatnot when we have them on the show, that’s who they speak to and loved ones. But from delving into all of this research about how schizophrenia treatment has evolved, my main takeaway is that it is a story about the medical community. It’s a story about individuals who shaped how schizophrenia was perceived and how it was to be managed. It’s not a story at all about the patients. It’s not even a story about schizophrenia in general. So much of what I found when it comes to the coma therapy, ECT, lobotomies, it all related to the physical aspects of what was done, and so many cases of abuse and all of the doctors and researchers and neurologists who came up with these things.
Rachel Star Withers: I never found anything that was, oh, water therapy was found to calm the symptoms of psychosis and schizophrenia and helped the patients regain a physical feeling of reality or patients of schizophrenia found an easier treatment that insulin therapy because they didn’t have to be injected with harmful chemicals. That’s not what was worded. And I feel that that’s what’s missing. You know, I don’t care as a schizophrenic who came up with the idea of sticking an ice pick through the eye. Lobotomies were successful 50% of the time, and some patients with schizophrenia voluntarily got multiple lobotomies, up to four. My question is, what made these patients want to go through it again? And I think as people who have schizophrenia and loved ones and the medical community, I think that’s really the important part. It’s people seeking to get better and learning to focus more on what helps these people, not just what calms all the people down and makes them controllable. I think it’s going to be a question that hopefully we’ll always be answering as we continue to evolve our treatments. I’m Rachel Star. Thank you so much for listening to this episode of Inside Schizophrenia. Wherever you downloaded this podcast, please subscribe. Also, take a moment to rate, rank and leave a written review so other people know why they should listen too. We’ll see everyone on the next episode of Inside Schizophrenia.
Announcer: Inside Schizophrenia is presented by PsychCentral.com, America’s largest and longest operating independent mental health website. Your host, Rachel Star Withers, can be found online at RachelStarLive.com. Co-host Gabe Howard can be found online at gabehoward.com. For questions, or to provide feedback, please e-mail talkback@PsychCentral.com. The official website for Inside Schizophrenia is PsychCentral.com/IS. Thank you for listening, and please, share widely.
Related Articles