Wearing a mask — any mask — reduces the risk of infection with the coronavirus, but wearing a more tightly fitted surgical mask, or layering a cloth mask atop a surgical mask, can vastly increase protections to the wearer and others, the Centers for Disease Control and Prevention reported on Wednesday.
New research by the agency shows that transmission of the virus can be reduced by up to 96.5 percent if both an infected individual and an uninfected individual wear tightly fitted surgical masks or a cloth-and-surgical-mask combination.
Dr. Rochelle P. Walensky, director of the C.D.C., announced the findings during Wednesday’s White House coronavirus briefing, and coupled them with a plea for Americans to wear “a well-fitting mask” that has two or more layers. President Biden has challenged Americans to wear masks for the first 100 days of his presidency.
“With cases hospitalizations and deaths still very high, now is not the time to roll back mask requirements,” she said, adding, “The bottom line is this: masks work and they work when they have a good fit and are worn correctly.”
Virus-related deaths, which resurged sharply in the United States in November and still remain high, appear to be in a steady decline; new virus cases and hospitalizations began to drop last month. But researchers warn that a more contagious virus variant first found in Britain is doubling roughly every 10 days in the United States. The C.D.C. cautioned last month that it could become the dominant variant in the nation by March.
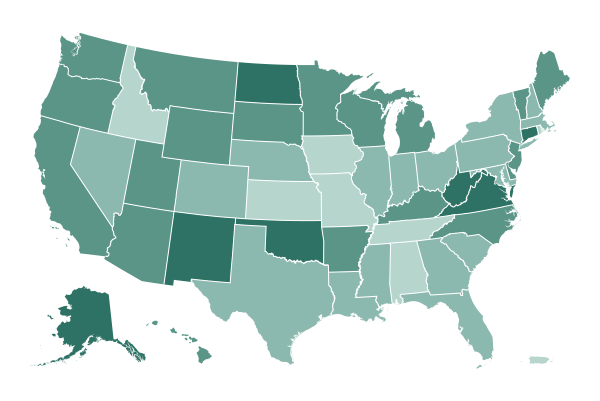
As of Feb. 1, 14 states and the District of Columbia had implemented universal masking mandates; masking is now mandatory on federal property and on domestic and international transportation. But while masks are known to both reduce respiratory droplets and aerosols exhaled by infected wearers and to protect the uninfected wearer, their effectiveness varies widely because of air leaking around the edges of the mask.
“Any mask is better than none,” said Dr. John Brooks, lead author of the new C.D.C. study. “There are substantial and compelling data that wearing a mask reduces spread, and in communities that adopt mask wearing, new infections go down.”
But, he added, the new research shows how to enhance the protection. The agency’s new laboratory experiments are based on the ideas put forth by Linsey Marr, an expert in aerosol transmission at Virginia Tech, and Dr. Monica Gandhi, who studies infectious diseases at the University of California, San Francisco.
One option for reducing transmission is to wear a cloth mask over a surgical mask, the agency said. The alternative is to fit the surgical mask more tightly on the face by “knotting and tucking” — that is, knotting the two strands of the ear loops together where they attach to the edge of the mask, then folding and flattening the extra fabric at the mask’s edge and tucking it in for a tighter seal.
Dr. Brooks cautioned that the new study was based on laboratory experiments, and it’s unclear how these masking recommendations will perform in the real world (the experiments used three-ply surgical and cloth masks).“But it’s very clear evidence that the more of us who wear masks and the better the mask fits, the more each of us benefit individually.”
Other effective options that improve the fit include using a mask-fitter — a frame contoured to the face — over a mask, or wearing a sleeve of sheer nylon hosiery material around the neck and pulled up over a cloth or surgical mask, the C.D.C. said.
Even as vaccines are being slowly rolled out across the country, the emergence of the new variants, which may respond differently to treatments or dodge the immune system to some degree, has prompted public health officials to emphasize that Americans should continue to take protective measures like masking.

Coronavirus-related deaths, which rose sharply in the United States beginning in November and remain high, appear to be in a steady decline, following in the tracks of new virus cases and hospitalizations, which began to drop last month.
The country has reported about 2,800 deaths a day recently, an average that excludes one anomalous day last week when Indiana announced a large number of backlogged death reports. That national average remains far above the level of early November, before the country’s recent surge, when roughly 825 deaths were being reported daily. But it is down significantly from the peak just a few weeks ago, when the average was more than 3,300 a day.
New coronavirus cases are a leading indicator for deaths, and that statistic has been improving markedly for a month. On Tuesday, the country reported 96,400 new cases, the third day in a row of having fewer than 100,000 new recorded cases, a level not seen since early November.
The seven-day average of new cases, a more reliable indicator of the pandemic’s direction, has fallen more than 50 percent since it peaked on Jan. 8.
Whether that will continue remains in doubt. Researchers warn that a more contagious virus variant first found in Britain is doubling roughly every 10 days in the United States. The Centers for Disease Control and Prevention cautioned last month that it could become the dominant variant in the nation by March.
Deaths tend to lag behind new cases by several weeks, and the day-to-day statistics can be prone to reporting vagaries. For a while, it was hard to discern clear signs that deaths had begun to decline. But the national trend now is unmistakable: The daily average has dropped about 18 percent since Jan. 12.
Although deaths are still rising in some states, including Alabama and South Carolina, far more are reporting sustained declines. Over the past two weeks, reports of virus deaths have dropped more than 40 percent in New Mexico and more than 30 percent in Arkansas, Colorado and Connecticut.
The declines are heartening but are not a reason for people to let down their guard, said Bill Hanage, an epidemiologist and associate professor at Harvard.
Dr. Hanage said the surges in new cases and deaths in December and early January had probably stemmed from the increase in gatherings over the holidays and from the onset of winter. Most kinds of coronavirus infections, including influenza, peak during winter, and there is little reason to think that Covid-19 is any different.
The more infectious nature of the Covid-19 virus, and the appearance of variants that may spread even more easily, remain a significant cause for caution, he said.
“If in response to these dropping numbers people relax, then it is entirely possible and expected that we will see that decline start to bottom out and even start to increase again,” he said.
A New York Times analysis found that about half of the country’s roughly 465,000 Covid-19 deaths have occurred since the brutal surge began in November.

Dozens of times a day in Covid-19 wards across California, a scene like this plays out: A hospital chaplain watches as a death is announced by machine.
Kristin Michealsen, a hospital chaplain in Los Angeles, stood at a man’s bedside, holding his hand. His relatives gathered at their home just minutes from the hospital — they were not allowed into the hospital ward. The patient’s heart had just stopped. Ms. Michealsen, an ordained minister, had watched a computer monitor as she accompanied the man to the edge of his life. Eighty beats per minute. Sixty. Forty.
California has averaged 433 daily deaths over the past week. On Tuesday, it became the state with the largest total toll, surpassing New York.
In the depersonalized math of the pandemic, there are two ways to view the ravages of the virus in California. As America’s most populous state, it has by far the most cases in the country — more than 3.4 million — and now the most deaths. But when adjusted for its large population, California has a lower death rate than 31 states and Washington, D.C.
With about 114 deaths per 100,000 people, the state has about half the rate of New York, New Jersey, Massachusetts or Mississippi. The disparity between New York and California could be even greater when taking into account the likelihood that New York undercounted deaths in the pandemic’s frenetic early stages because virus testing was so limited.
Yet these mitigating statistics mean little to the families of the more than 44,900 people killed by the virus in California. Nor do the numbers mean much to chaplains like Ms. Michealsen, who on that day in January when the picture was taken by an Associated Press photographer had already watched two other patients die. Often, she is the only other person in the room when death comes. Sometimes, a nurse holds the other hand of the dying patient.
“When we come into this world, we are immediately surrounded by people — we have human touch,” Ms. Michealsen said last week from the Providence Holy Cross Medical Center in Los Angeles. “I just think that when we leave this world, we should have the same.”
The pandemic has taken an uneven toll in California, with people in the south and agricultural Central Valley much harder hit than those in the north.
In San Francisco, where almost 350 people have died from the virus, the cruelty of the pandemic — the inability of families to surround their dying relatives, the interruption of age-old rituals of mourning — is wearing.
“I’ve never in 15 years experienced the multiple layers of loss that we are experiencing now,” said Naomi Tzril Saks, a chaplain at the University of California, San Francisco medical center. Like chaplains across the country, Ms. Saks and her colleagues have done what they can to remedy the cruel isolation of the disease.
“We’ve Zoomed in bands and people playing the violin,” Ms. Saks said. “We Zoomed in a person’s son who was incarcerated, and she hadn’t seen him for years before she died.”
Chaplains have gone on virtual retreats to avoid emotional burnout, Ms. Saks said. Some have joined national support groups.
“There are stories and experiences from this pandemic that will stay in my body for a very long time,” Ms. Saks said.

After a two-week pause of in-person instruction, the Chicago Teachers Union said early Wednesday that its members had approved an agreement to reopen classrooms in the country’s third-largest public school system.
More than 20,000 ballots were cast, with 13,681 members voting in favor and 6,585 voting against, the union said.
Under the agreement, prekindergarten and some special education students will return to classrooms on Thursday. Staff in kindergarten through fifth-grade classrooms will return on Feb. 22, and students in those grades will return on March 1. Staff members in sixth- through eighth-grade classrooms will return March 1, and students on March 8.

Listen to ‘The Daily’: What Will It Take to Reopen Schools?
The Biden administration is determined to restart in-person learning quickly. But there are some major hurdles.
“This plan is not what any of us deserve,” Jesse Sharkey, the president of the Chicago Teachers Union, said in a statement. “This agreement represents where we should have started months ago, not where this has landed.”
“We will protect ourselves by using the school safety committees created under this agreement to organize and see that C.P.S. meets safety standards and mitigation protocols,” Mr. Sharkey said. “Safety Committees will enforce this agreement, have access to information and the ability to change unsafe practices in their school.”
Ms. Sharkey criticized Mayor Lori Lightfoot over her handling of the situation and said that union delegates had passed a vote of no confidence in the mayor and school leadership on Monday night.
Ms. Lightfoot and the chief executive of the district, Janice K. Jackson, said in a statement, “This vote reaffirms the strength and fairness of our plan, which provides families and employees certainty about returning to schools and guarantees the best possible health and safety protocols.”
Ms. Lightfoot, a Democrat, and the union have been locked in one of the most intense disagreements over reopening anywhere in the country. The mayor has argued that the city’s most vulnerable students need the opportunity to return to school in person, while the union condemned the city’s reopening plan as unsafe.

The theory was compelling: Could children be less vulnerable to the new coronavirus because they carry antibodies to other coronaviruses that cause the common cold? Might that also help explain why some people infected with the new virus have mild symptoms while others are more severely affected?
The notion gained traction particularly among people who thought it would swiftly bring about herd immunity. A study in the journal Science, published in December, gave the hypothesis a strong boost.
But a new study published on Tuesday in the journal Cell found that the theory does not hold up. Based on experiments with live virus and with hundreds of blood samples drawn before and after the pandemic, the research refutes the idea that antibodies to seasonal coronaviruses have any impact on the new coronavirus, called SARS-CoV-2.
“Going into this study, we thought we would learn that individuals that had pre-existing, pre-pandemic antibodies against SARS-CoV-2 would be less susceptible to infection and have less severe Covid-19 disease,” said Scott Hensley, an immunologist at the University of Pennsylvania. “That’s not what we found.”
He and his colleagues concluded that most people are exposed to seasonal coronaviruses by age 5. As a result, about one in five people carries antibodies that recognize the new coronavirus.
But the team found that these antibodies are not neutralizing — they cannot disarm the virus, nor do they mitigate the severity of symptoms after infection.

A top European Union official said on Wednesday that the bloc was “not where we want to be” in handling the pandemic, after missteps in lining up vaccine supplies left it lagging behind other countries.
“We were late to authorize,” the official, Ursula von der Leyen, the president of the European Commission, the bloc’s executive arm, told lawmakers in Brussels.
“We were too optimistic when it came to massive production, and perhaps too confident that what we ordered would actually be delivered on time,” she said. “We need to ask ourselves why that is the case.”
She stood by the view that buying vaccine doses as a bloc had been the right decision, however.
“I cannot even imagine what would have happened if just a handful of big players — big member states — had rushed to it and everybody else would have been left empty-handed,” she said, adding that it would have been “the end of our community.”
Her comments came as criticism has mounted over Ms. Von der Leyen’s handling of negotiations with pharmaceutical companies to secure vaccines for the 450 million people living in the bloc’s 27 member states.
Whereas Britain and United States have surged ahead in rolling out vaccines, the European Union has been more cautious and price-conscious, leading to a crisis after vaccine producers said there were delays in filing orders.
Its tensions with Britain, which left the bloc’s authority at the end of last year, were magnified after the Commission reversed an attempt last month to restrict vaccine exports into the country via Northern Ireland.
“The bottom line is that mistakes were made in the process leading up to the decision,” Ms. von der Leyen said on Wednesday. “And I deeply regret that. But in the end, we got it right.”
Over 17 million people, or about 4 percent of people living in the bloc, have received at least one vaccine dose, she said.

There is a growing and glum sense in France that its efforts to quell the pandemic have stalled. The country is caught between a slow-moving vaccine rollout and infection rates that remain high despite months of restrictions.
Last month, the country was bracing for a third nationwide lockdown when President Emmanuel Macron unexpectedly decided against it. He made a calculated gamble that he could tighten restrictions just enough to stave off a new surge of cases while avoiding the heavier economic and social toll of more drastic measures like those in force in Britain and Germany.
Weeks later, it is still unclear whether that bet will pay off or whether, as some health experts have warned, there is little chance of containing the spread without a strict lockdown.
The average number of daily infections, at about 20,000, has neither spiked nor fallen much over the past month. Hospitalizations are stable but still at high levels. And more contagious variants from other parts of the world are spreading.
More than 2.2 million out of France’s population of 67 million have received at least one vaccine dose, and nearly 250,000 have been fully inoculated. But with 3.1 doses administered per 100 people, according to a New York Times database, France still trails neighbors like Italy and Spain.
Arnaud Fontanet, an epidemiologist at the Institut Pasteur who is a member of the government’s Covid-19 advisory council, said last weekend that the chances of containing the epidemic without a tight lockdown were thin.
“Everything will depend on our ability to control the spread of the British variant,” Mr. Fontanet told the Journal du Dimanche newspaper.
“There is a lot of wavering,” said Odile Essombé-Missé, 79, who was standing in line at a vaccination center in Pontoise for her 85-year-old husband’s injection. Asked about a new lockdown, she shrugged.
“We put up with it,” she said. Her eyeglasses, perched atop a colorful blue and orange face mask, were fogged over.

The U.S. Food and Drug Administration on Tuesday granted emergency use authorization to a Covid-19 therapy that combines two monoclonal antibody drugs.
The approval of the treatment, which is manufactured by the drug maker Eli Lilly, gives doctors another option for patients with Covid-19 who are not sick enough to be hospitalized but are at high risk of becoming seriously ill. Such therapies received a publicity boost under President Donald Trump when he and several other politicians took them while sick with Covid-19, but the drugs have not been widely used in many places, even as hospitalizations soared through the fall and into the winter.
Researchers are hopeful about suggestions in preliminary data that the new combination therapy may be better able to fight virus variants compared with a similar treatment already in use.
The therapy combines the company’s drug known as bamlanivimab — which was authorized in November and is being used for high-risk Covid-19 patients — with a second drug known as etesevimab. Both consist of artificially synthesized copies of the antibodies generated naturally when an immune system fights off infection.
Another monoclonal antibody combination therapy, made by Regeneron, is also authorized in the United States.
In clinical trial results announced last month, high-risk patients with Covid-19 who were given Eli Lilly’s combination therapy were significantly less likely to end up hospitalized than those who received a placebo. No patients who were given the combination therapy died.
The combination therapy must be given via an intravenous infusion. On Tuesday, the F.D.A. said that bamlanivimab alone could now be infused for a period as short as 16 minutes, down from an hour when the therapy was first authorized.
That long infusion time is one reason that monoclonal antibody drugs have not been more widely used in some places. Patients and their families have also struggled to gain access to the therapies. Some hospitals have been too overwhelmed to prioritize the drugs. And some doctors have been hesitant to embrace them, saying that they want to see more evidence from clinical trials supporting the drug’s use.
Global Roundup

Vacationing abroad may not be possible for residents of Britain until all adults in the country have been vaccinated, a government official said on Wednesday, raising questions about how the tourism industry might cope with such restrictions and dashing hopes of many who hoped that a relatively successful vaccine rollout in Britain could let them enjoy trips abroad this summer.
The transportation secretary, Grant Shapps, said on British television that international travel would depend on “everybody having their vaccinations” in Britain, and that restrictions could remain as long as other countries have not made significant progress in vaccinations.
“We’ll need to wait for other countries to catch up as well, in order to do that wider international unlock,” Mr. Shapps said.
As of Wednesday, Britain had administered more than 12.5 million vaccine doses, equivalent to about 18 percent of its population, one of the highest rates in the world. At the current pace, the country is on track to give the first shot of a two-dose coronavirus vaccine to its entire population by the end of June.
The authorities have reported a sharp drop in the number of infections in recent days, and Prime Minister Boris Johnson is expected to announce a potential loosening of restrictions this month.
But on Wednesday, Mr. Shapps urged caution about travel plans for this year and advised people not to book vacations either within Britain or abroad. “I’m afraid I can’t give you a definitive ‘will there or will there not be’ the opportunity to take holidays,” he told Sky News.
Mr. Shapps’s warning came a day after the authorities announced new travel restrictions, including prison sentences of up to 10 years for anyone traveling to Britain who lies about where they’ve been.
Mr. Shapps called the measures, including the jail sentence, “appropriate.” Under other restrictions that are set to come into force on Monday, British residents arriving in England from more than 30 countries where coronavirus variants are believed to be widespread, will have to pay up to 1,750 pounds ($2,410) for a 10-day quarantine in government-managed hotel rooms.
Britain has reported 114,000 deaths from the coronavirus, the world’s fifth-highest known death toll.
In other developments around the world:

As Major League Baseball players gear up for spring training, the league and the players’ union agreed late Monday to new health and safety obligations built on some of the regulations and pandemic lessons from 2020’s baseball season.
The operations manual governing the 2021 Major League Baseball season is 108 pages and regulates coronavirus protocols. It includes a five-day quarantine before reporting to spring training; shorter spring training games; no indoor dining; mandatory wearable contact-tracing devices; and discipline for violations, including for failure to wear a mask correctly, or at all, while at the stadium.
Before the delayed and abbreviated 60-game 2020 season began, M.L.B. and the union agreed to a similarly lengthy operations manual. But back then they were entering uncharted waters. Now, they have the benefit of their own experience and the knowledge of what worked for other sports.
The rules may still evolve as they did last season. Initial delays with the every-other-day testing were ironed out. And after two early outbreaks on the St. Louis Cardinals and the Miami Marlins threatened the season’s viability, M.L.B. tightened its protocols and became more aggressive in postponing games after a positive test, while players and key workers became more vigilant.
In the end, all but two teams — the Detroit Tigers and the Cardinals — played the full 60 games in the regular season. There wasn’t a positive test among players for nearly two months. The creation of bubblelike conditions allowed the postseason to go off without a hitch — until the final day, when Justin Turner returned to the field to celebrate the Los Angeles Dodgers’ World Series title despite having been pulled from the game after a positive test.
“I’m cautiously optimistic,” Dr. Michael Saag, an infectious diseases expert at the University of Alabama at Birmingham who is not affiliated with M.L.B. or the union, said about 2021’s protocols in a telephone interview on Tuesday. “I think the mitigation rules that they’ve created now have evidence that it worked for the most part, with a few exceptions.”