Roy Lakes wasn’t planning to get a coronavirus shot until he overheard a Zumba instructor urging her attendees to sign up. “You owe it to your kids, to your grandkids, to stay around,” the instructor kept saying.
Those words changed his mind. The 46-year-old from Anaheim, Calif., who has worked as a mental health counselor, has now set up an appointment with his doctor to discuss getting vaccinated.
Health-care workers were the first group in the United States to be offered coronavirus vaccinations. But three months into the effort, many remain unconvinced, unreached and unprotected. The lingering obstacles to vaccinating health-care workers foreshadows the challenge the United States will face as it expands the pool of people eligible and attempts to get the vast majority of the U.S. population vaccinated.
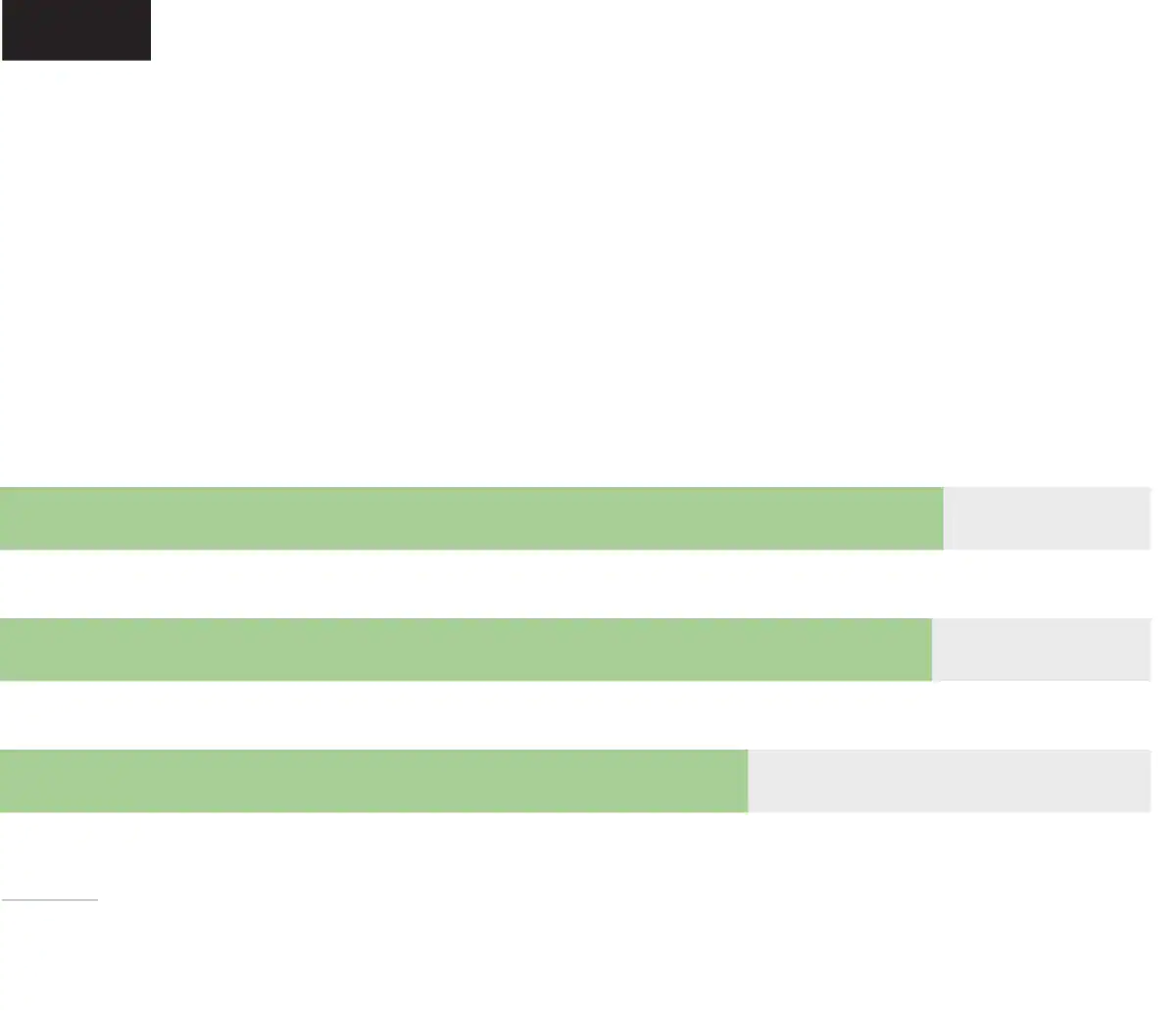
According to a Washington Post-Kaiser Family Foundation poll, barely half of front-line health-care workers (52 percent) said they had received at least their first vaccine dose at the time they were surveyed. More than 1 in 3 said they were not confident vaccines were sufficiently tested for safety and effectiveness.
The nationally representative survey of 1,327 front-line health-care workers, conducted Feb. 11 through March 7, illustrates the challenges ahead as vaccine advocates try to persuade a wider population — with less familiarity with medicine — to get vaccinated.
While about 2 in 10 health-care workers said they had scheduled a shot or were planning to, 3 in 10 health-care workers said they were unsure about getting vaccinated or not planning to do so. As many as 1 in 6 health workers said that if employers required them to get vaccinated, they would leave their job.
[Read the Post-KFF poll results and how the survey was conducted]
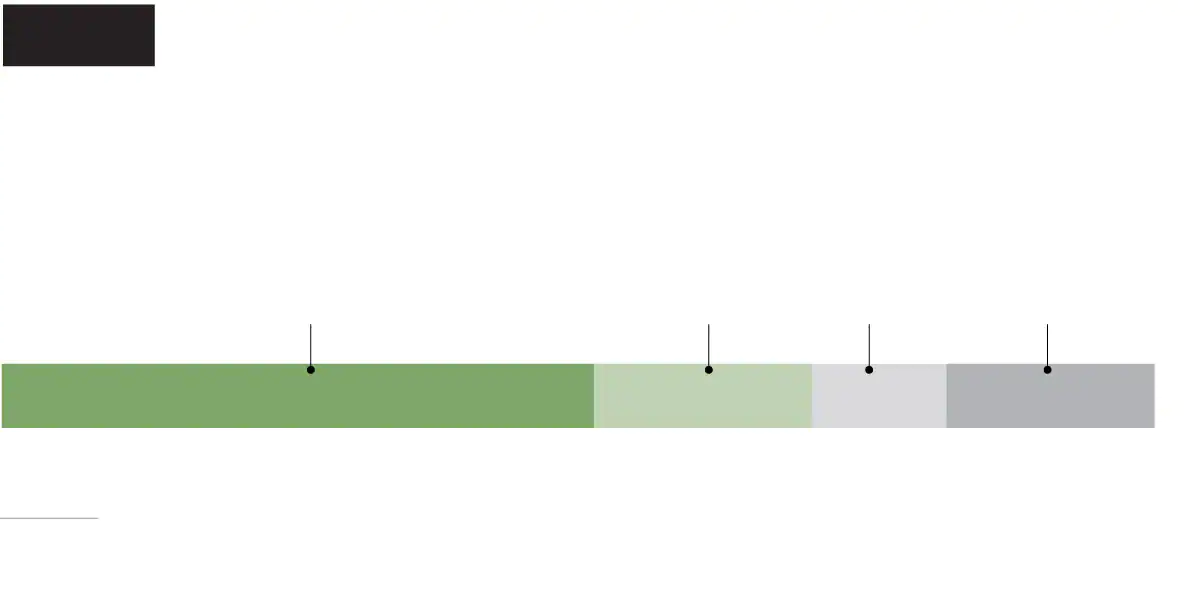
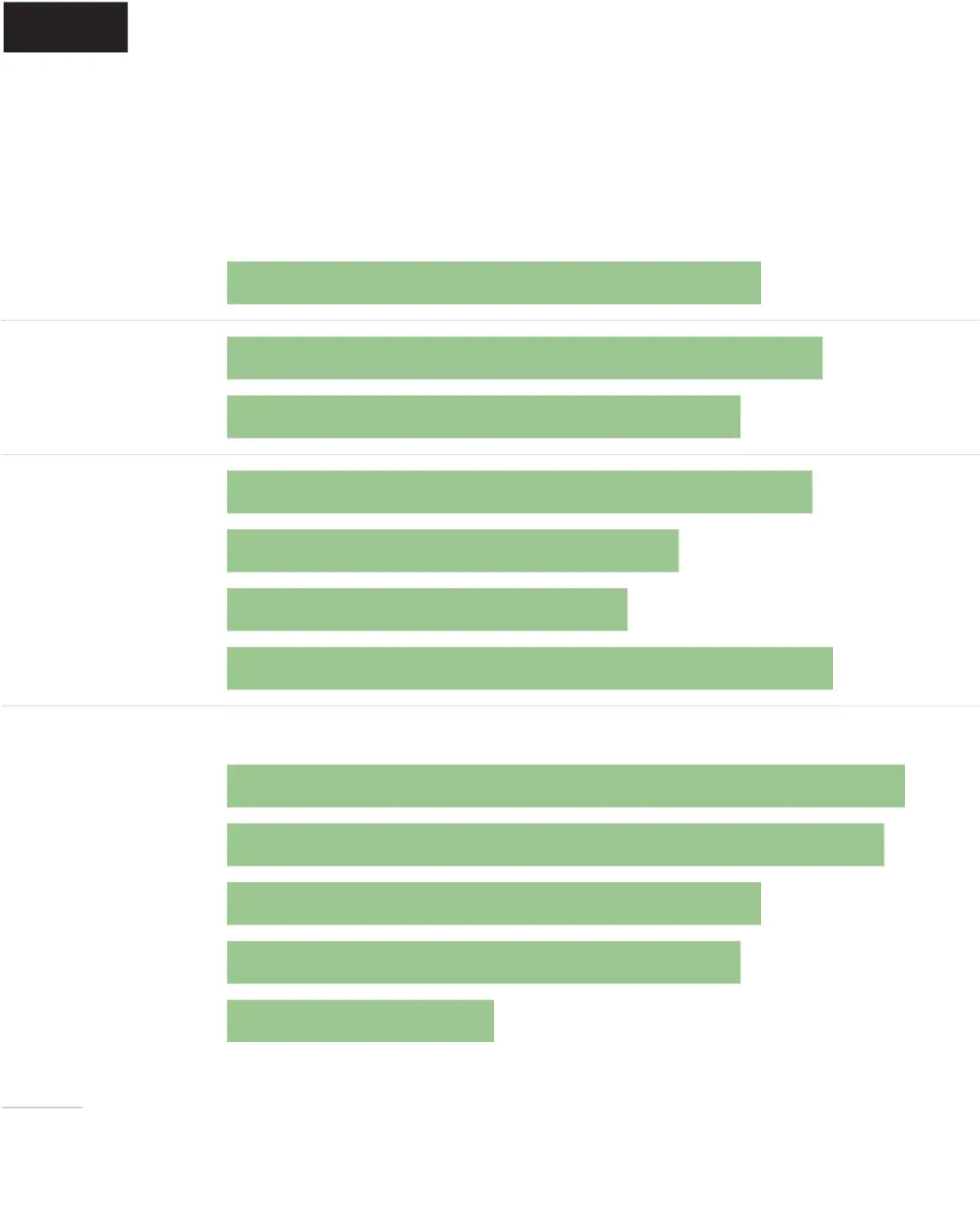
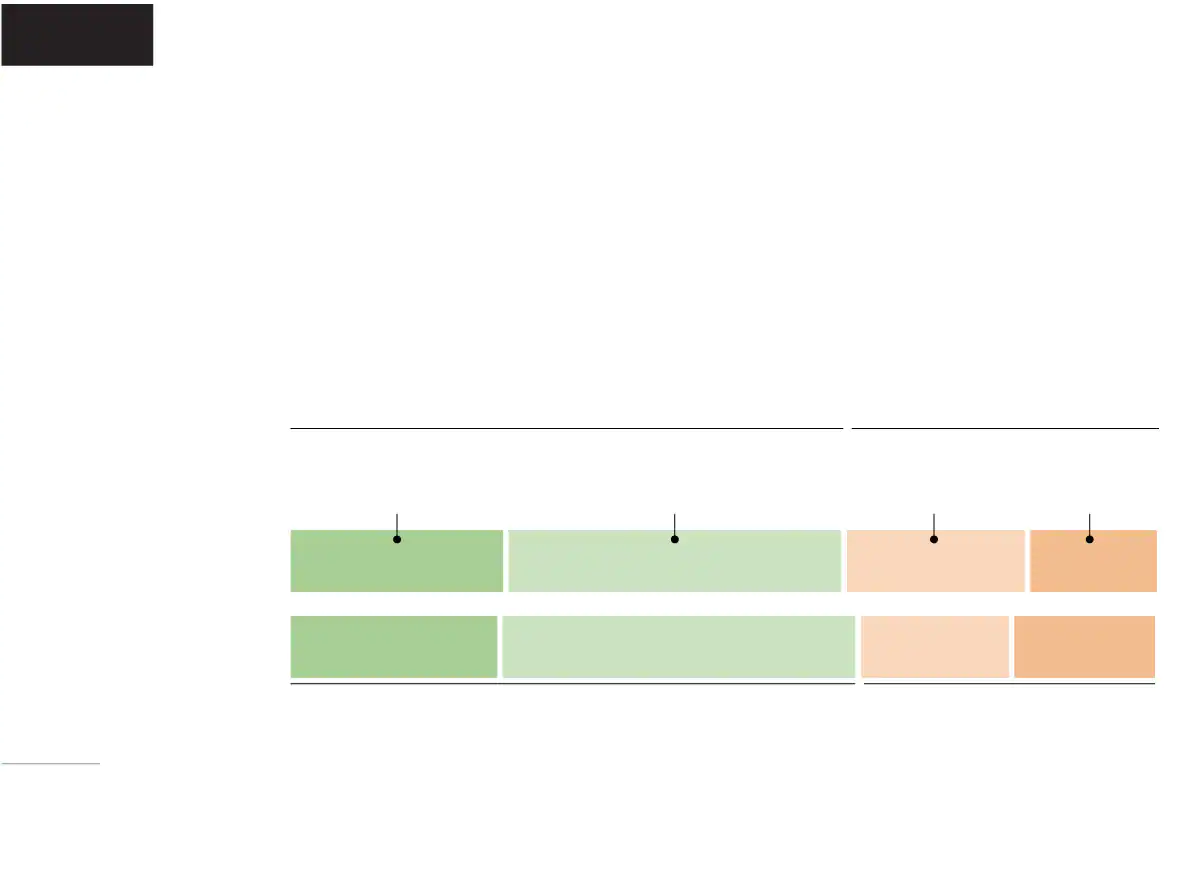
Washington Post- Kaiser
Family Foundation poll
Many health-care workers have yet to get a coronavirus shot, and some don’t plan to
Vaccinated (at least 1 dose)
Don’t plan on being vaccinated
Note: No opinion not shown.
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3 percentage points.

Washington Post-Kaiser Family
Foundation poll
Many health-care workers have yet to get a coronavirus shot, and some don’t plan to
Vaccinated (at least 1 dose)
Don’t plan on being vaccinated
Note: No opinion not shown.
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3 percentage points.
Washington Post-Kaiser Family Foundation poll
Many health-care workers have yet to get a coronavirus
shot, and some don’t plan to
Don’t plan
on being
vaccinated
Vaccinated
(at least 1 dose)
Note: No opinion not shown.
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3 percentage points.
Washington Post-Kaiser Family Foundation poll
Many health-care workers have yet to get a coronavirus
shot, and some don’t plan to
Vaccinated
(at least 1 dose)
Don’t plan on
being vaccinated
Note: No opinion not shown.
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3 percentage points.
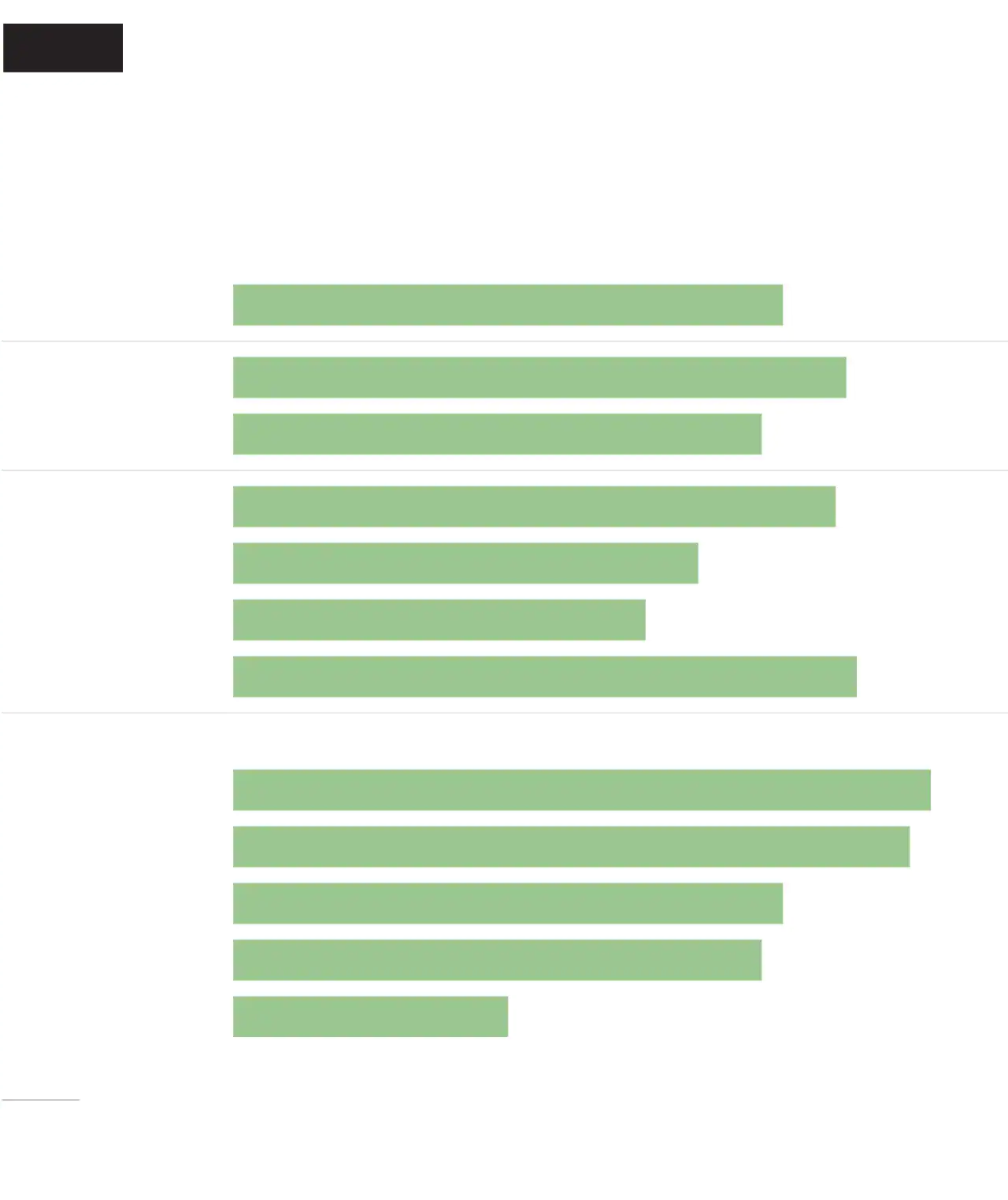
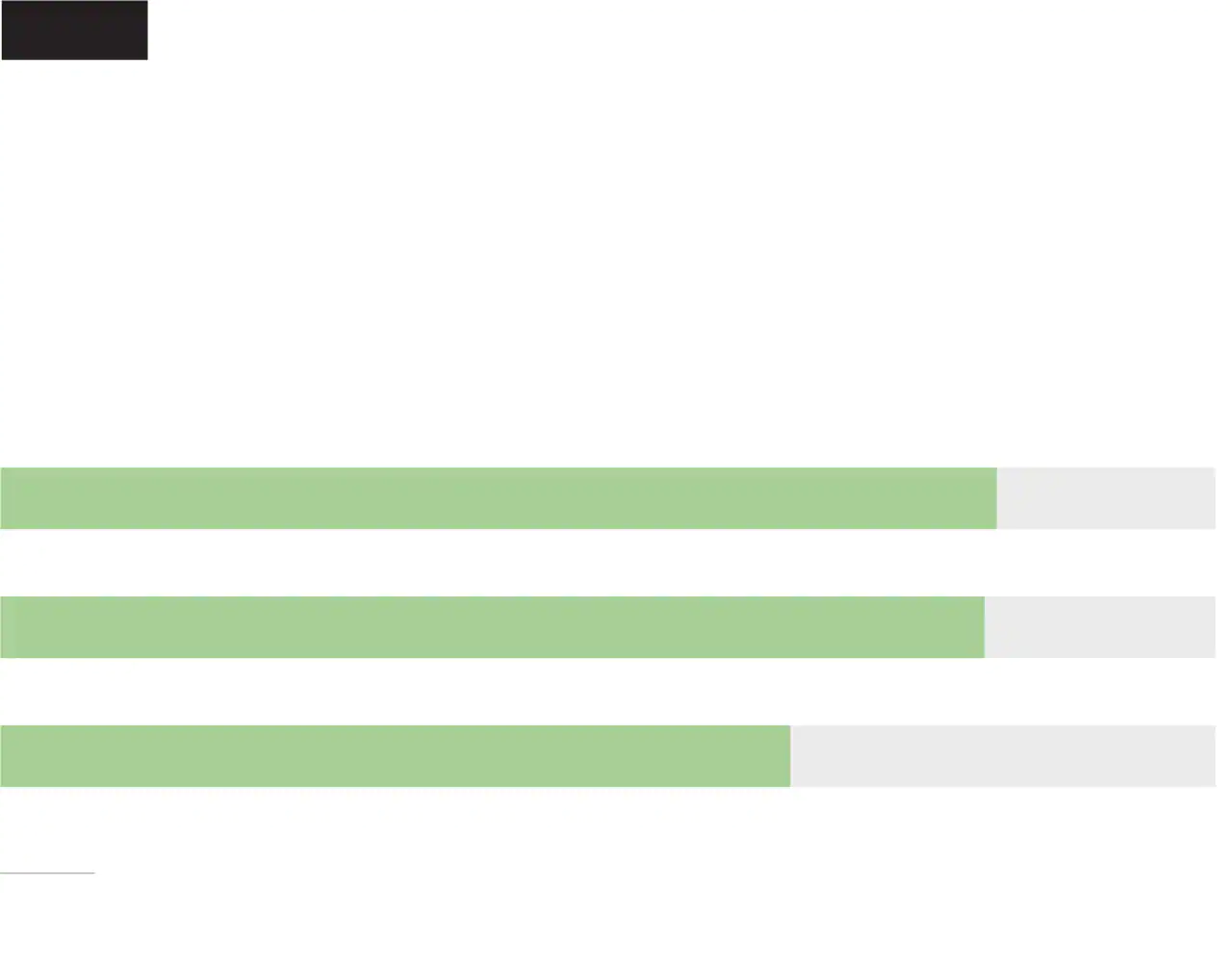
Vaccination rates are particularly low among health-care workers who are Black, those in lower-paying jobs such as home health aides and those with less education. Partisan politics also play a role, with more Democrats saying they have been vaccinated and Republicans more likely to express uncertainty or concerns about the vaccines.
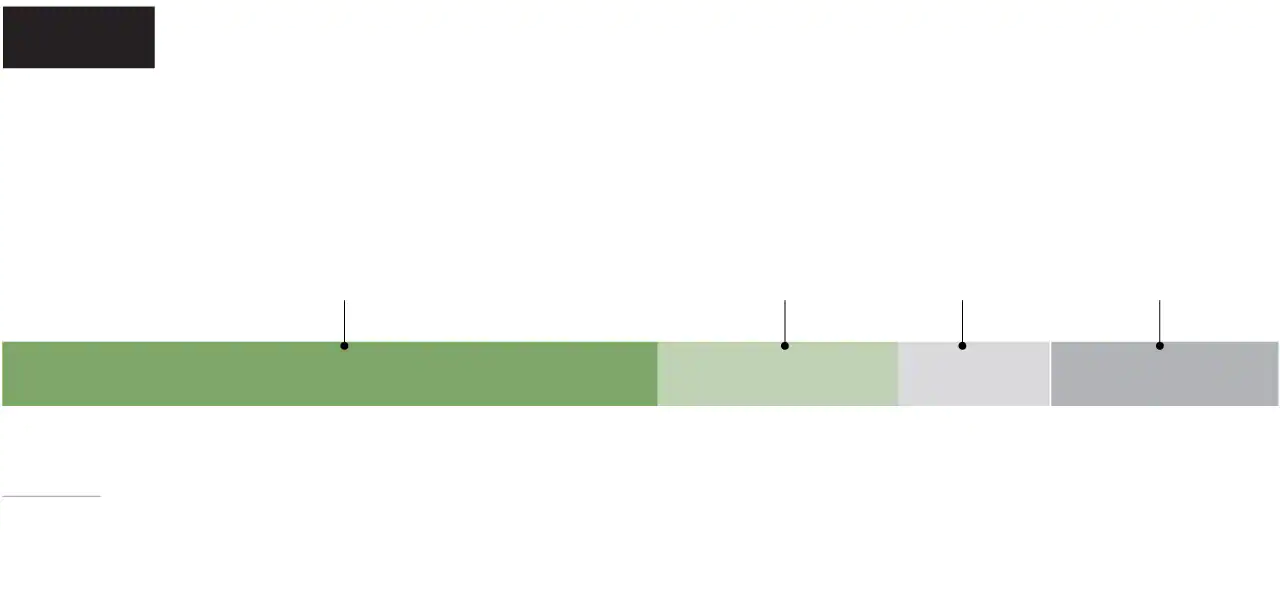
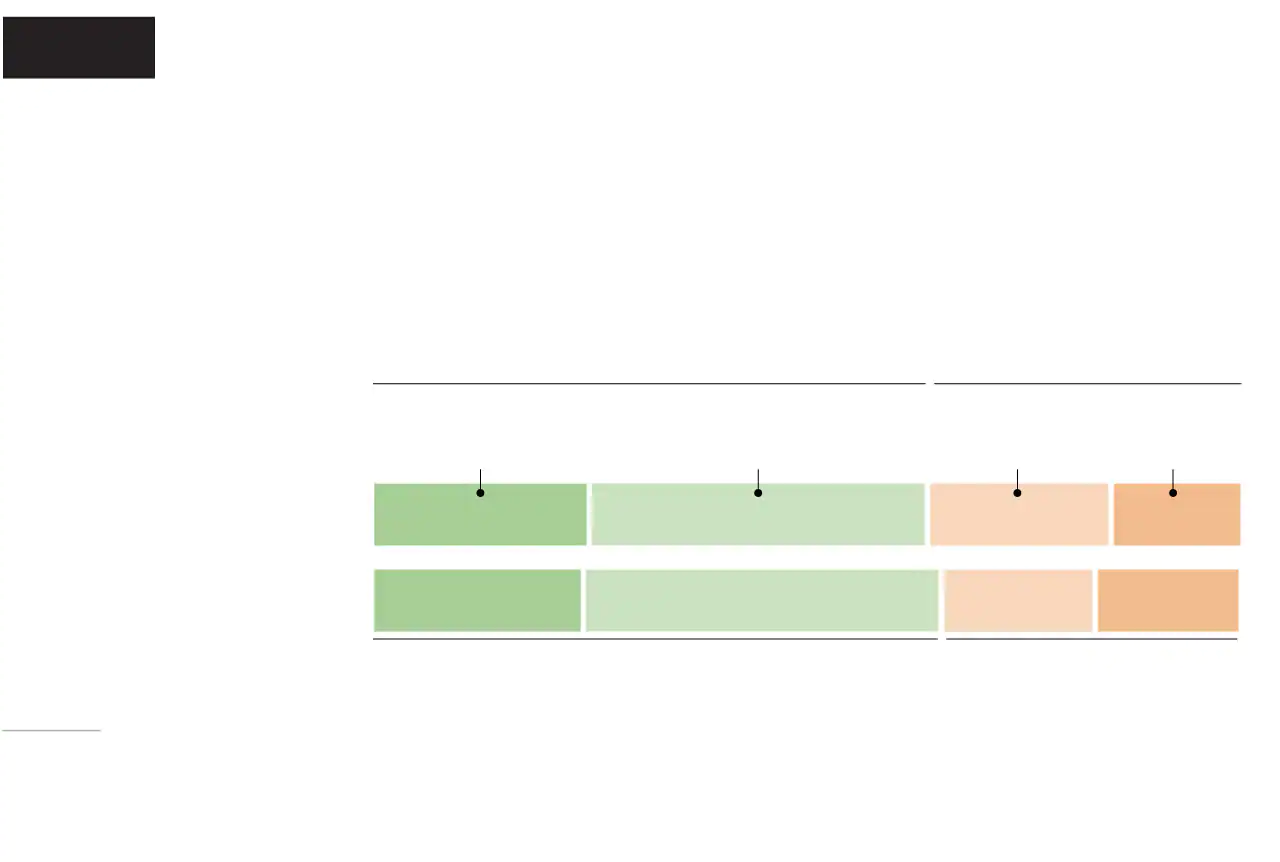
Washington Post- Kaiser
Family Foundation poll
Vaccination rates lowest among
Black health-care workers,
women and those working
in patients’ homes
Q: Have you personally received at least one dose of a covid-19 vaccine?
Received at least one dose
Health-care
workers overall
Nursing home/
Assisted care
facility
Note: Not all response options shown.
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3 percentage points. Error margins higher among subgroups.
Washington Post-Kaiser Family
Foundation poll
Vaccination rates lowest among Black
health-care workers, women and those
working in patients’ homes
Q: Have you personally received at least one dose of a covid-19 vaccine?
Received at least one dose
Health-care
workers overall
Nursing home/
Assisted care facility
Note: Not all response options shown.
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3 percentage points. Error margins higher among subgroups.
Washington Post-Kaiser Family Foundation poll
Vaccination rates lowest among Black health-care workers
women, and those working in patients’ homes
Q: Have you personally received at least one dose of a covid-19 vaccine?
Received at least one dose
Health-care
workers overall
Nursing home/
Assisted care facility
Note: Not all response options shown.
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3 percentage points. Error margins higher among subgroups.
Washington Post-Kaiser Family Foundation poll
Vaccination rates lowest among Black health-care workers, women
and those working in patients’ homes
Q: Have you personally received at least one dose of a covid-19 vaccine?
Received at least one dose
Health-care
workers overall
Nursing home/
Assisted care facility
Note: Not all response options shown.
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error
margin of +/- 3 percentage points. Error margins higher among subgroups.
“Health-care workers are everybody,” said Bruce Gellin, president of global immunization at the Sabin Vaccine Institute. Gellin noted that the hesitancy and disparities encompass a range of health workers, from front-line infectious-disease doctors who followed the vaccine science and approval process carefully to home health aides who may have little access to such specialized knowledge — or to the shots — in their work settings.
The Post-KFF survey is the most comprehensive survey of vaccine adoption across the health-care workforce, encompassing those working in hospitals, assisted-living facilities, patient’s homes and other health-care delivery settings. Other studies echo the findings. A Centers for Disease Control and Prevention study found that by mid-January, 38 percent of staffers at long-term care facilities in the agency’s vaccination program had received a first dose. Becker’s Hospital Review found that among eight top-rated hospitals, between 63 percent and 84 percent of employees had received at least one dose by mid-February.
The new vaccines were shipped immediately after receiving emergency use authorization from the federal government. And because health-care workers were the first to be offered vaccinations, some took a wait-and-see approach.
“There was very little time to prepare health-care workers for the vaccines,” said Kelly Moore, deputy director of the Immunization Action Coalition, which promotes vaccine education.
Now that more than 75 million people have been vaccinated, with very few side effects and broad-based national educational campaigns being launched to counter concerns, experts hope vaccine confidence will increase among health-care workers and others.
Swaying those minds toward vaccination will determine how quickly and completely the United States is able to bring the crisis phase of the pandemic to an end.
“Unless we all do it together, we’re not going to be victorious over the virus,” Gellin said.
‘I don’t think there is enough research’
The more people are vaccinated in the coming weeks, the closer the country will come to herd immunity, slowing the ability of the virus to transmit. But if large groups of the population never get vaccinated, the virus will continue circulating and mutating.
Even among health-care workers — who have seen the devastation of the virus up close and work in a field rooted in science — 36 percent expressed doubts about the safety and efficacy of the vaccines, a rate that closely mirrors that of the general public.
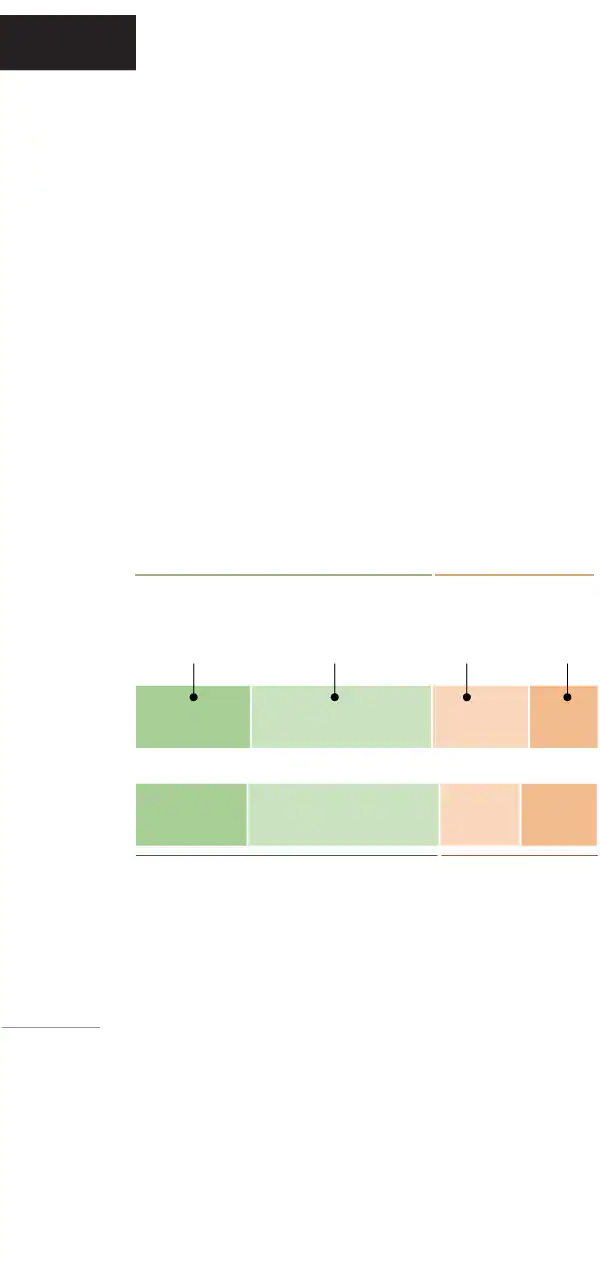
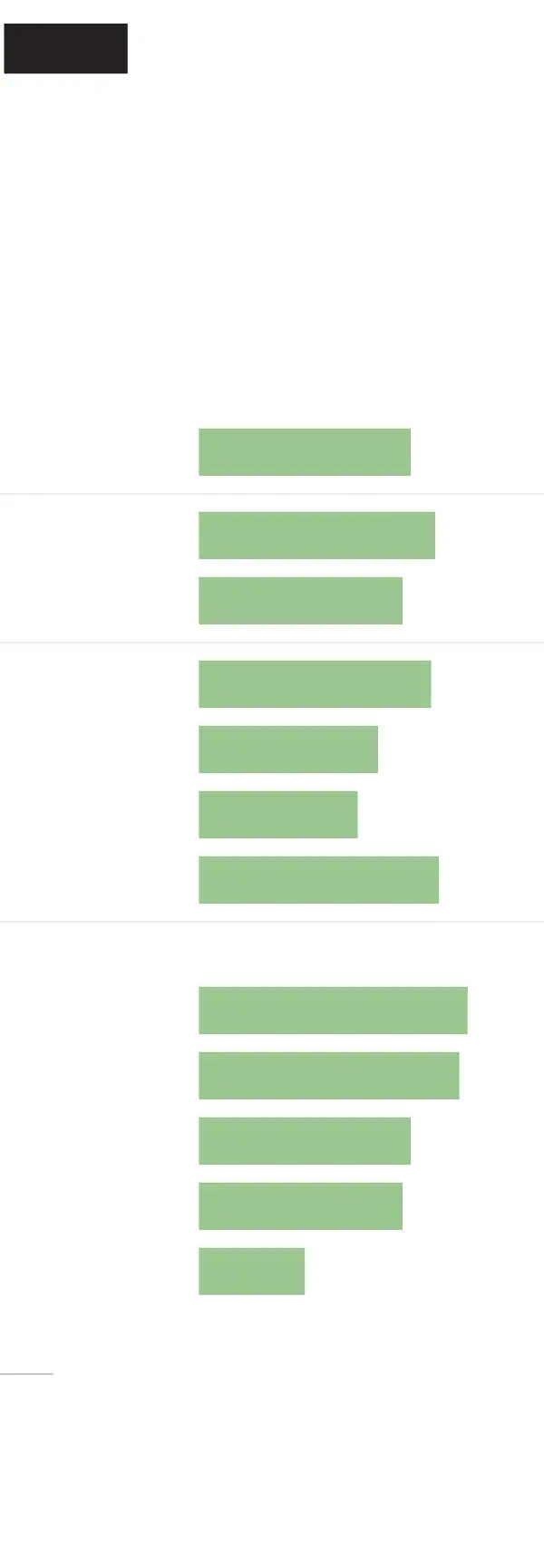
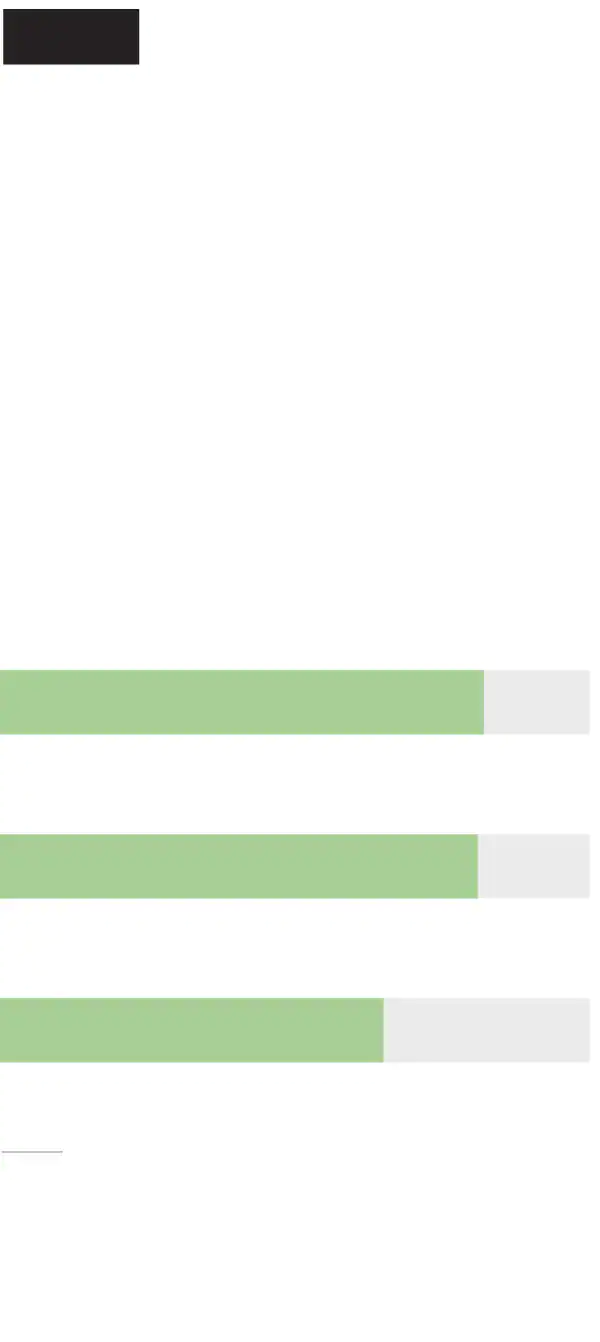
Washington Post- Kaiser
Family Foundation poll
As with the American general public, nearly two-thirds of U.S. health-care workers express confidence in vaccine safety and effectiveness
Q: How confident are you that the covid-19 vaccines in the U.S. have been properly tested for safety and effectiveness?
Note: No opinion not shown.
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error margin of +/- 3 percentage points and 971 U.S. adults with an error margin of +/- 4 points. Because of rounding, numbers do not always
add up to 100.
Washington Post-Kaiser Family
Foundation poll
As with the American general public, nearly
two-thirds of U.S. health-care workers
express confidence in vaccine safety
and effectiveness
Q: How confident are you that the covid-19 vaccines in the U.S. have been properly tested for safety and effectiveness?
Note: No opinion not shown.
Source: Post-KFF survey of 1,327 U.S. health-care workers from
Feb. 11 to March 7, 2021, with an error margin of +/- 3
percentage points and 971 U.S. adults with an error
margin of +/- 4 points. Because of rounding,
numbers doOOOnot always add up to 100.
Washington Post-Kaiser Family Foundation poll
As with the American general public, nearly two-thirds of U.S. health-care workers express confidence in vaccine safety
and effectiveness
Q: How confident are you that the covid-19 vaccines in the U.S. have been properly tested for safety and effectiveness?
Note: No opinion not shown.
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an
error margin of +/- 3 percentage points and 971 U.S. adults with an error margin of +/- 4 points.
Because of rounding, numbers do not always add up to 100.
Washington Post-Kaiser Family Foundation poll
As with the American general public, nearly two-thirds of U.S. health-care
workers express confidence in vaccine safety and effectiveness
Q: How confident are you that the covid-19 vaccines in the U.S. have been properly tested for safety and effectiveness?
Note: No opinion not shown.
Source: Post-KFF survey of 1,327 U.S. health-care workers from Feb. 11 to March 7, 2021, with an error
margin of +/- 3 percentage points and 971 U.S. adults with an error margin of +/- 4 points. Because of
rounding, numbers do not always add up to 100.
While individuals’ explanations for that hesitancy vary, they often revolve around three core ideas: safety, efficacy and trust.
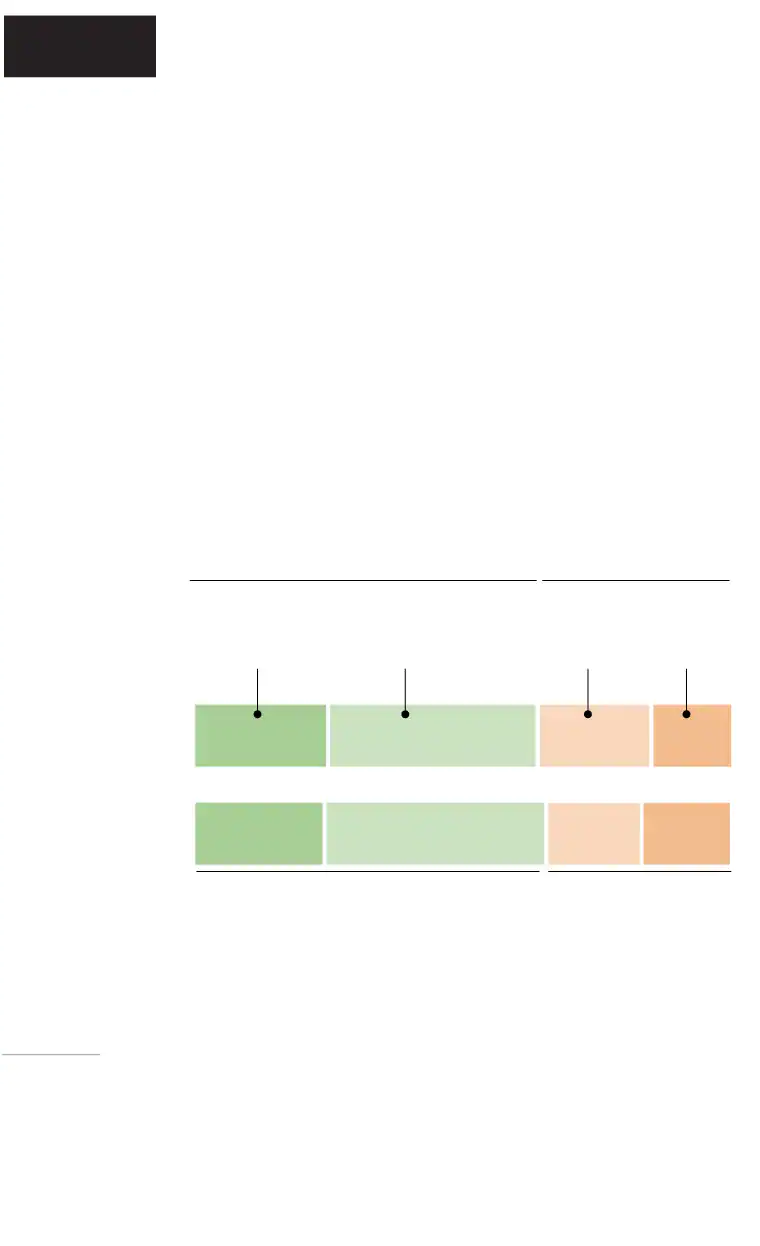
About 8 in 10 health-care workers who were not planning to get vaccinated against coronavirus or were on the fence said they were waiting to see how the vaccine affects others and were worried about adverse side effects. About two-thirds of those unvaccinated and without plans to get vaccinated said they did not trust the government to ensure the safety of the coronavirus vaccines.
Rather than considering the critical mass of vaccinated people needed for herd immunity, people are often thinking on an individual level and want an answer to a simple question, Gellin said: “Are people like me taking this vaccine, and how are they doing?”
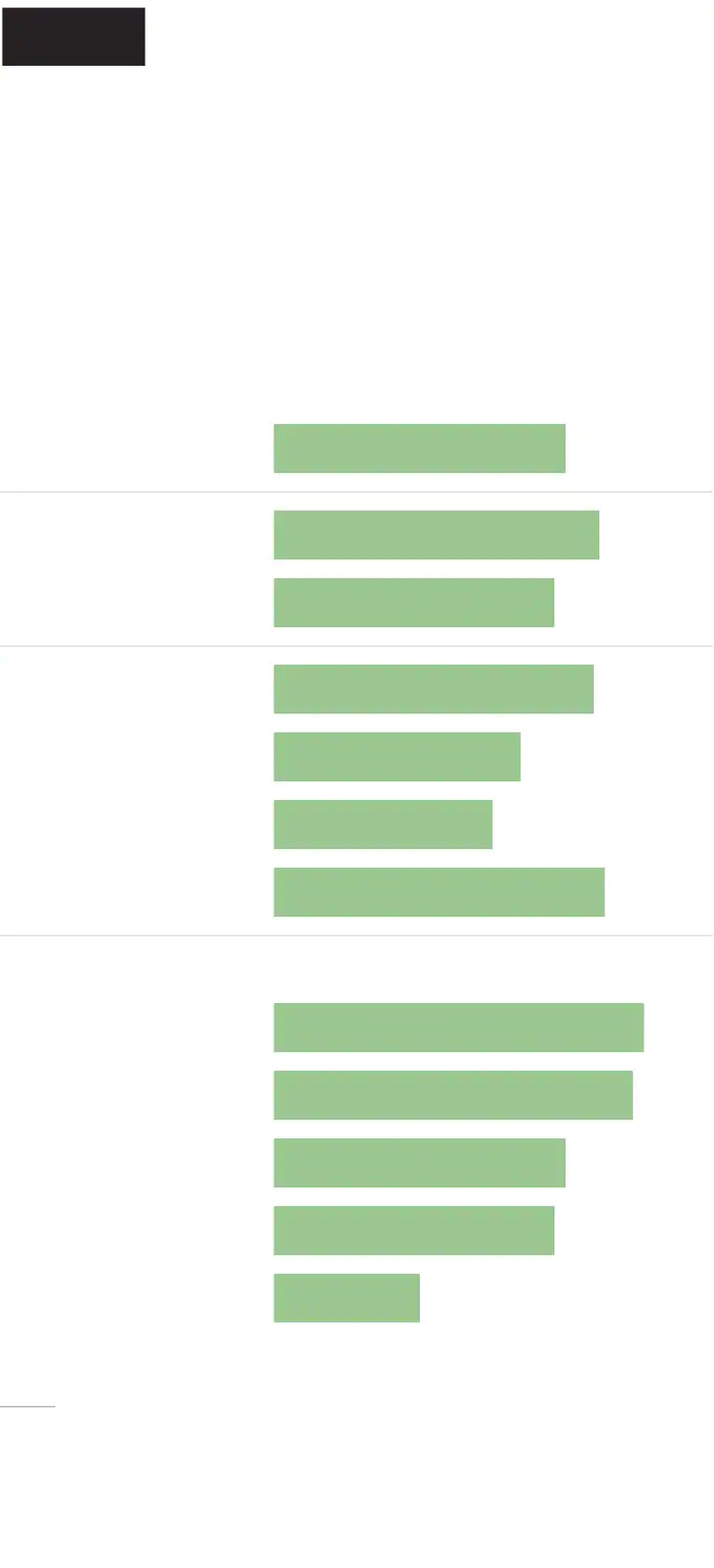
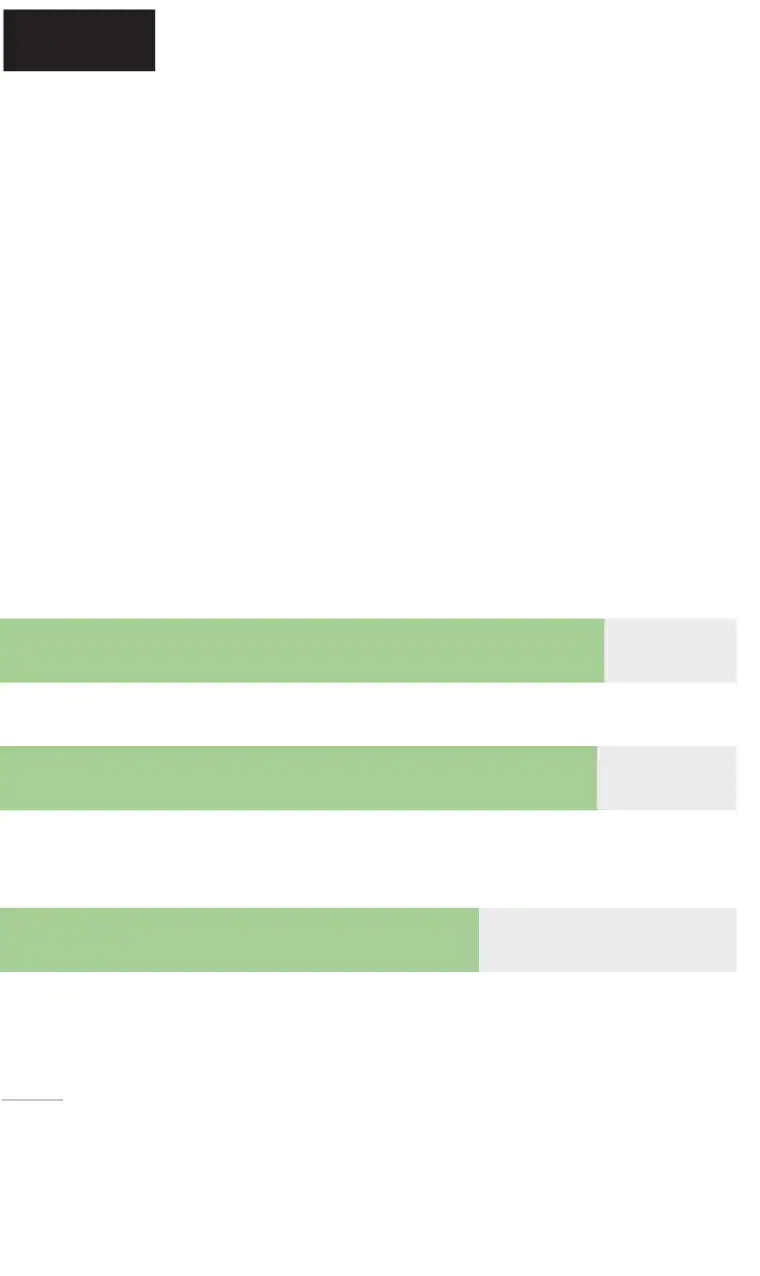
Washington Post- Kaiser
Family Foundation poll
Unvaccinated health-care workers
say waiting to see how it works
for others and side effects are
biggest factors in their decision
Q: Is each of the following a major factor in your decision on whether to get a covid-19 vaccine, a minor factor, or not a factor?
Among unvaccinated health-care
workers who are unsure or do not
plan to get vaccinated
Worried about possible side effects
Want to wait and see how vaccines
work for other people
Do not trust the government to make sure
the vaccine is safe and effective
Note: Not all response options shown.
Source: Post-KFF survey from Feb. 11 to March 7, 2021, of 365 U.S. health-care workers who are unsure about getting vaccinated or do not
plan to do so, with an error margin of
+/- 6 percentage points.
Washington Post-Kaiser Family
Foundation poll
Unvaccinated health-care workers say
waiting to see how it works for others
and side effects are biggest
factors in their decision
Q: Is each of the following a major factor in your decision on whether to get a covid-19 vaccine, a minor factor, or not a factor?
Among unvaccinated health-care workers who are
unsure or do not plan to get vaccinated
Worried about possible side effects
Want to wait and see how vaccines work for other people
Do not trust the government to make sure
the vaccine is safe and effective
Note: Not all response options shown.
Source: Post-KFF survey from Feb. 11 to March 7, 2021, of
365 U.S. health-care workers who are unsure about getting vaccinated or do not plan to do so, with an error margin of
+/- 6 percentage points.
Washington Post-Kaiser Family Foundation poll
Unvaccinated health-care workers say waiting to see how it works
for others and side effects are biggest factors in their decision
Q: Is each of the following a major factor in your decision on whether to get a covid-19 vaccine, a minor factor, or not a factor?
Among unvaccinated health-care workers who are unsure
or do not plan to get vaccinated
Worried about possible side effects
Want to wait and see how vaccines work for other people
Do not trust the government to make sure the vaccine is safe and effective
Note: Not all response options shown.
Source: Post-KFF survey from Feb. 11 to March 7, 2021, of 365 U.S. health-care workers who
are unsure about getting vaccinated or do not plan to do so, with an error
margin of +/- 6 percentage points.
Washington Post-Kaiser Family Foundation poll
Unvaccinated health-care workers say waiting to see how it works for
others and side effects are biggest factors in their decision
Q: Is each of the following a major factor in your decision on whether to get a covid-19 vaccine, a minor factor, or not a factor?
Among unvaccinated health-care workers who are
unsure or do not plan to get vaccinated
Worried about possible side effects
Want to wait and see how vaccines work for other people
Do not trust the government to make sure the vaccine is safe and effective
Note: Not all response options shown.
Source: Post-KFF survey from Feb. 11 to March 7, 2021, of 365 U.S. health-care workers who are unsure
about getting vaccinated or do not plan to do so, with an error margin of +/- 6 percentage points.
Shelly Robinson, a long-term care nurse in Upstate New York, said she sees many covid-19 patients but does not want to risk getting a shot, because she feels the vaccines were rushed.
“I don’t think there is enough research,” Robinson said.
Many elderly patients have gotten vaccinated, she said, to be reunited with family members. But for now, she intends to rely on her mask for protection.
“I’m going to wait,” Robinson said. “Me and my family will keep wearing the masks until there are more studies done.”
One of the starkest numbers from the poll shows that 16 percent of health-care workers would rather give up their jobs than get vaccinated. The poll finds 58 percent of health-care workers who are not self-employed support their employer requiring all workers to be vaccinated. Among Americans who are not health workers, 70 percent say people who work with patients should be required to get a coronavirus vaccine.
“I’d quit if work told me I had to take it,” said Sandy Hull, 65, a registered nurse who lives just outside Indianapolis. She works in a prison and in a behavioral health setting for adolescents. “I wouldn’t run the risk of ruining my health to continue working.”
Hull said she believes the coronavirus exists and that she takes general precautions such as washing her hands and wearing a mask, but she said she believes that the virus’s dangers have probably been exaggerated because of political and financial concerns.
“It seems to me if it was as contagious as they say, I would have probably ended up catching it,” Hull said.
[‘We want to be educated, not indoctrinated,’ say Trump voters wary of covid shots]
Even though many health-care employers require influenza vaccines, Moore, of the Immunization Action Coalition, warned against enforcing coronavirus vaccination as a term of employment — at least for now.
“Mandates can be counterproductive” unless they follow extensive confidence-building programs that are designed to address employees’ concerns, she said.
“They come after, not instead of, educational efforts,” she said.
 A health-care worker gets a dose of the Pfizer-BioNTech vaccine in Miami in December. (Marco Bello/Reuters)
A health-care worker gets a dose of the Pfizer-BioNTech vaccine in Miami in December. (Marco Bello/Reuters) ‘I was so glad to get the shot’
The Post-KFF poll finds sharp income and educational differences in vaccination rates of health-care workers. More than 7 in 10 health-care workers with postgraduate degrees had received at least their first dose, compared with over 6 in 10 of those with bachelor’s degrees and 4 in 10 of those with an associate’s degree or less.
Some health-care workers cannot access the vaccine, even if they want to get it.
Samuel Charles Jr., 67, handles intake of patients at a primary-care doctor’s office in Chicago, taking their temperature and paperwork. Despite the high volume of patients he interacts with, Charles does not know why he was never offered a coronavirus vaccine through his job or his status as a health-care worker.
It was only because he was in the University of Chicago’s hospital’s system as a former patient that he was vaccinated at the end of February. Suffering from chronic obstructive pulmonary disease, he almost died in 2019 and spent two weeks in an intensive care unit. The hospital called and offered him a shot, given his underlying conditions.
“I guess I was lucky in that sense. If I hadn’t almost died, I wouldn’t have been on their list for the vaccine,” Charles said. “I was so glad to get the shot.”
The income disparity among health-care workers is clear. Nearly 7 in 10 health-care workers with household incomes of $90,000 and above said they had been vaccinated. But that dropped to about half of those with incomes between $40,000 and $90,000 and to roughly 3 in 10 of those with incomes even lower than that.
Michael Kauten, 59, has been wanting to get vaccinated for months. Even before the first vaccine was approved in December, he said, he would have been willing to get it. He worked a lower-paying health-care job in a long-term care facility for adults with disabilities, but by the time some health-care workers were starting to get vaccinated at the end of December, cutbacks brought on the pandemic resulted in Kauten getting laid off.
Still, working as a volunteer firefighter in Wisconsin, Kauten should have been able to get a shot as a first responder, but his deeply rural department still has not received a supply.
It wasn’t until a few days ago that he learned he could sign up for the shot at a local drugstore such as Walgreens, he said. No one told him, and he was too busy struggling to find a new job.
“I had no idea,” Kauten said. He recently was hired as a long-term substitute teacher at a local school and is scheduled through the school department to get a shot at the end of the month.
[Tracking the coronavirus vaccine]
 Health-care workers wait in line to get vaccinated at the Fairfax County Government Center in Virginia on Jan. 2. (Michael S. Williamson/The Washington Post)
Health-care workers wait in line to get vaccinated at the Fairfax County Government Center in Virginia on Jan. 2. (Michael S. Williamson/The Washington Post) The Post-KFF poll underscores the importance of employers providing vaccinations to health-care workers. Nearly 8 in 10 of those who said they had been vaccinated received doses from their employers. Hospitals have been most effective, with 66 percent of those who work directly with patients in hospitals receiving at least one dose, compared with 50 percent of those working in nursing homes or assisted-care facilities, 39 percent of those who are self-employed and 26 percent of those working in patients’ homes. Just over half of those who work in doctors’ offices said they had been vaccinated (52 percent).
Among health workers who planned to get vaccinated but had yet to make an appointment, just over 6 in 10 said they planned to do so through their employer, though roughly 3 in 10 said their employer had not offered them a shot.
Access is one of the key variables in people’s decision about whether to go through with getting a vaccine, experts say. When people are on the fence, having easy, convenient access can often tip the balance toward vaccination.
“We don’t need every person to be a champion, just comfortable enough to choose to be vaccinated,” Moore said. That means making sure the actual process of vaccination is convenient, considering factors such as work schedules and child-care needs.
‘I was a lot more comfortable’
Partisanship matters when it comes to vaccination, with 48 percent of Republican or Republican-leaning health workers saying they had received at least one dose, compared with 58 percent of Democrats. Over a third of Republican health workers, 36 percent, said they were uncertain or did not plan to get vaccinated, compared with 21 percent of those identifying or leaning Democratic.
Race is one of the strongest predictors of vaccine disparities.
The Post-KFF poll finds that 57 percent of White health-care workers, 39 percent of Black health-care workers and 44 percent of Hispanic health-care workers said they had been vaccinated.
 Nurse Sandra Lindsay, who in December was the first U.S. recipient of a coronavirus vaccination after the Pfizer-BioNTech vaccine was approved for public use, gets her second dose in Queens in early January. (Shannon Stapleton/Pool/Getty Images)
Nurse Sandra Lindsay, who in December was the first U.S. recipient of a coronavirus vaccination after the Pfizer-BioNTech vaccine was approved for public use, gets her second dose in Queens in early January. (Shannon Stapleton/Pool/Getty Images) Overall, 53 percent of health-care workers say they have been encouraged by their colleagues to get vaccinated. But only 4 in 10 Black health-care workers say they have been encouraged by their colleagues to get vaccinated, compared with over half of White health-care workers and just over 6 in 10 Hispanic health-care workers.
Robinson, who is Black, said the government’s history of mistreatment of minorities — including the infamous “Tuskegee Study of Untreated Syphilis in the Negro Male” in 1972, in which Black men with syphilis were left untreated — is one reason Black Americans remain skeptical of coronavirus vaccines.
[Biden’s vaccine push runs into distrust in the Black community]
Lorena Esquivel, 28, a patient access representative at San Ysidro Health in Southern California, worried initially that not enough time had been given to clinical trials. Access to colleagues who were ready to answer questions was key to her decision to get vaccinated.
“All that knowledge. After that, I was a lot more comfortable,” said Esquivel, who is Hispanic and has received both doses.
“Even after being vaccinated, there’s a possibility I can still get the virus,” Esquivel said. “I’m not immune. Patients feel like they are immune and they are not. The vaccine helps prevent them ending up in the hospital.”
 Health-care workers call a car forward this month at a mass vaccination site set up at Martinsville Speedway in Ridgeway, Va. (Andrew Caballero-Reynolds/AFP/Getty Images)
Health-care workers call a car forward this month at a mass vaccination site set up at Martinsville Speedway in Ridgeway, Va. (Andrew Caballero-Reynolds/AFP/Getty Images) ‘It is the only way we will get to the end of this pandemic’
James Conway, 47, knows several co-workers who remain scared of getting the vaccine, and he has wanted to change their minds. Conway works as a respiratory therapist at a hospital in St. Louis and has seen up close for the past year the death and suffering caused by the virus.
“It is the only way we will get to the end of this pandemic,” Conway said. But he has been careful not to press too hard or get into debates with co-workers.
“It’s like the patients I work with, you can’t force the respiratory therapy on them,” he said. “Approaching it that way is futile.” Instead, he often tells patients about his struggles with asthma and how such therapies have helped him.
Similarly, he has been asking co-workers about their vaccine doubts and trying to listen to them without judgment. And he ends those conversations making sure that they know that he got the vaccine and that he has not had an adverse reaction.
“I think that’s more persuasive than getting into argument,” Conway said. “For a lot of people, the only thing that will change their mind is time. Once they see others are fine and nothing went wrong, they will be more willing.”
For Lakes, at 46-year-old from Anaheim, thinking of his children made him want to get vaccinated. He spent 12 years working as a mental health counselor before the pandemic forced him to stop working.
“I would hate for my kids to be cursing me at my grave for not taking it,” he said.
[After months of trauma, vaccinated health-care workers welcome a surprising emotion: Hope]
The Post-KFF poll finds more than 9 in 10 vaccinated health-care workers said they experienced minor side effects (60 percent) or no side effects (34 percent). Among the 6 percent reporting “major side effects,” the most common were similar to those found in clinical trials: aches and pain, tiredness, headache, fevers or chills. A separate January study found that across 17.5 million doses given in December and January, just 66 resulted in severe allergic reactions, none of which resulted in death.
 A health-care worker in West Chester, Pa., prepares a dose of the Moderna vaccine in December. (Matt Slocum/AP)
A health-care worker in West Chester, Pa., prepares a dose of the Moderna vaccine in December. (Matt Slocum/AP) Mindy Darling, a nurse practitioner in Arizona who works in three nursing homes, said she devoted time to reading up about the research and listening to experts.
Darling, 38, who is White, says she is now passing on that information. She recalled an informal gathering with nurses and patients pulling up in wheelchairs, when she discussed the potential for long-haul covid-19, as opposed to the short-term side effects of a vaccine.
After the conversation, the assistant director of nursing came over. “That’s a good point about the effects of the disease,” Darling recalled her saying.
Darling was pleased to see that people in leadership positions plastered the walls of one facility with a simple poster listing their names.
“We are taking the covid vaccine,” it read. “Ask us why.”
Addressing health-care workers’ concerns is particularly important, Moore said, because they tend to wield great influence with their families and friends, as well as with their patients.
“Fix this problem and it’s going to be better for everyone,” Moore said.
Scott Clement contributed to this report.





